A Guide to Cell Signaling in Cancer Development and Progression
How To Guide
Published: September 7, 2023
Regardless of cell type, the tumorigenic changes that drive cancer growth and metastasis are complex. Decoding these cellular changes and identifying the associated molecular pathways is key to the discovery of novel therapeutic targets for the next generation of cancer treatments .
This guide highlights some of the key pathways that are commonly dysregulated in cancer. It also explores how dysregulation can lead to pathogenesis with examples across a broad range of cell and tissue types.
Download this guide to discover:
- Illustrated examples of cellular changes commonly associated with the hallmarks of cancer
- Key therapeutic targets and their context within cell signaling pathways
- The latest tools to accelerate your cancer research
Oncology guide
Cellular signaling processes involved in cancer development and progression
Oncology Guide - Cellular signaling processes involved in cancer development and progression
2 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Molecular drivers of cancer pathogenesis
Cancer progression is associated with the interplay between tumor cells and
the surrounding environment, which requires signal transduction pathways
to relay messages throughout the cell.1,2 Cell signaling pathways regulate
everything from cell growth to proliferation to survival. PI3K/AKT/mTOR and
Ras/MAPK are examples of the main pathways that are interconnected and
mediate signals from receptor tyrosine kinases (RTKs) to intracellular effector
proteins and cell cycle regulators.3
The growth of breast, ovarian, and prostate
cancers depend on the proliferative signal induced by their hormones since
they express hormonal receptors.4
Many of these pathways are altered in
cancer and contribute to cancer progression.3
Genetic or epigenetic alterations in tumor cells are often the underlying cause
of cancer. Genetic alterations to cellular genes may be inherited or arise
spontaneously because of DNA damage from an environmental carcinogen
or mutation from replication errors.1
Many common genetic lesions in cancer
involve signaling proteins. These mutations can either activate genes or result
in loss of function. Hyperactivation of these pathways drives tumorigenesis
and supports tumor growth.2
Signaling pathway proteins that are commonly
activated by physiological responses include growth factor receptor (e.g.
EGFR), small GTPases (e.g. Ras), serine/threonine kinases (e.g. Raf and
Akt), cytoplasmic tyrosine kinases (e.g. Src and Abl), lipid kinases (e.g.
phosphoinositide 3-kinases, PI3Ks), as well as nuclear receptors (e.g. the
estrogen receptor). The components of developmental signaling pathways
such as Wnt, Hedgehog, Hippo, and Notch can also be altered. Finally,
downstream nuclear targets of signaling pathways like the transcription
factors Myc and NF-κB, chromatin remodelers, and cell cycle effectors are
also commonly altered. Many of the genes commonly mutated encode
Purpose and scope
INTRODUCTION
components or targets of the PI3K/AKT and Ras/ERK pathways, causing
dysregulation of cellular signaling.1
This dysregulation drives cancer progression by influencing the behavior
of tumor cells through cell proliferation, survival, migration, differentiation,
metabolism, polarity, angiogenesis, and the tumor microenvironment.
Why this guide?
Cancer is a complex entity and regardless of cancer type, there are frequently
observed cellular changes involved in tumorigenesis, tumor growth, and
metastasis. Decoding these cellular changes and correlating to molecular
pathways are key to novel discoveries that will help develop the next
generation of cancer treatments. This guide highlights a selection of the
key events and pathways that are dysregulated and lead to pathogenesis.
Discover scientific background and illustrations covering cellular changes
associated with many of the hallmarks of cancer.
References
1. Sever R, Brugge JS. Signal Transduction in Cancer. Cold Spring Harbor Perspectives in Medicine. 2015;5(4).
doi:10.1101/cshperspect.a006098
2. Benjamin D. Cancer Signaling Pathways and Crosstalk. Accessed August 8, 2022. https://www.mdpi.com/
journal/cancers/special_issues/Cancer_Signaling_Pathways_and_Crosstalk
3. Yip HYK, Papa A. Signaling Pathways in Cancer: Therapeutic Targets, Combinatorial Treatments, and New
Developments. Cells. 2021;10(3):659. doi:10.3390/cells10030659
4. Sanchez-Vega F, Mina M, Armenia J, et al. Oncogenic Signaling Pathways in The Cancer Genome Atlas. Cell.
2018;173(2):321-337.e10. doi:10.1016/j.cell.2018.03.035
Oncology Guide - Cellular signaling processes involved in cancer development and progression
3 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
The initiation and development of cancer is driven by a disruption in the
balance of multiple cellular processes. In cancer cells, mutations in genes
that control the cell cycle lead to errors in division, suppression, and death.
Whether it’s the disruption of defective cell clearing or an imbalance between
self-renewal and differentiation, mutations within these processes that drive
the modification of proteins and their associated signaling pathways can
ultimately result in tumorigenesis. As cell proliferation increases, there are
also associated metabolic changes that result in increased glucose uptake
and lactate production that further promote tumor growth. Much research
goes into elucidating basic biological processes that drive the early stages
of cancer and its growth, with early-stage treatment being the best course
of action for a patient. Identifying inhibitors that can mitigate the various
imbalances within some of the key processes highlighted in this guide is an
ongoing focus of oncology drug discovery.
Introduction
DRIVERS OF TUMORIGENESIS AND TUMOR GROWTH
x x x
Drivers of Tumor Growth
Altered Metabolism in Cancer Cell
Cytoplasm
Mitochondrion
Extracellular space
Reduced oxidative
phosphorylation
PI3K
Pyruvate Increased anaerobic
glycolysis
Acidic
microenvironment
Lactate
Lactate Glucose
Myc
HIF
HIF
HIF
LDHA
CO2
AKT
mTOR
Loss of tumor
suppressor function
Decreased mitochondria
activity and O2 consumption
LDHA and glucose
transporter expression MXI 1 COX4
Mutated
p53
Mutated
PTEN
Citric
acid
cycle
Altered Cell Death Signalling in Cancer Cell
Cytoplasm
Nucleus
Extracellular space
PI3K RTK TNF receptor
Cytochrome C
Apoptosis
Autophagy
Downregulated or
mutated TNF
receptors reduce
apoptosis
Dysregulated
PI3K/AKT pathway
AKT
Caspase 3 Caspase 8
Complex
1
DISC
NFKB
NFKB
mTOR FADD
Bax
Bak
Pro-survival gene
expression, e.g.
Bcl-X2 Altered Proliferation in Cancer Cell
Cytoplasm
Nucleus
Extracellular space
RTK
PI3K RAS RAF MEK
ERK
CDK2
RB
RB E2F
E2F
mTOR
AKT
Gene
transcription
Cell cycle
Dysregulated cell cycle
Faulty DNA repair mechanisms
Mitochondrion
Cyclin D
Cyclin E
CDK
4/6
M
G1
G2
S
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression 4 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
x
x
x
Drivers of Tumor Growth
Altered Metabolism in Cancer Cell
Cytoplasm
Mitochondrion
Extracellular space
Reduced oxidative
phosphorylation
PI3K
Pyruvate Increased anaerobic
glycolysis
Acidic
microenvironment
Lactate
Lactate Glucose
Myc
HIF
HIF
HIF
LDHA
CO
2
AKT
mTOR
Loss of tumor
suppressor function
Decreased mitochondria
activity and O2 consumption
LDHA and glucose
transporter expression MXI 1 COX4
Mutated
p53
Mutated
PTEN
Citric
acid
cycle
Altered Cell Death Signalling in Cancer Cell
Cytoplasm
Nucleus
Extracellular space
PI3K RTK TNF receptor
Cytochrome C
Apoptosis
Autophagy
Downregulated or
mutated TNF
receptors reduce
apoptosis
Dysregulated
PI3K/AKT pathway
AKT
Caspase 3 Caspase 8
Complex 1
DISC
NFKB
NFKB
mTOR FADD
Bax
Bak
Pro-survival gene
expression, e.g.
Bcl-X2 Altered Proliferation in Cancer Cell
Cytoplasm
Nucleus
Extracellular space
RTK
PI3K RAS RAF MEK
ERK
CDK2
RB
RB E2F
E2F
mTOR
AKT
Gene
transcription
Cell cycle
Dysregulated cell cycle
Faulty DNA repair mechanisms
Mitochondrion
Cyclin D
Cyclin E
CDK
4/6
M
G1
G2
S
Oncology Guide - Cellular signaling processes involved in cancer development and progression
5 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Genes control the cell division process and regulate a balance between
promoting cell proliferation, suppressing it, and inducing cellular death
(apoptosis). In cancer, mutations lead to a disruption of this balance that
results in unchecked cell growth. This results in unchecked cell growth.1 The
cause of cancer cell overgrowth is complex and often involves many different
genes in different types of cancer.2
Normal cell growth is tightly regulated in a series of coordinated events that
take place during the cell division cycle. In response to signals from growth
factors (mitogens), chromosomes are replicated once in the S phase and
segregated to create two genetically identical daughter cells in the mitosis or
M phase. Growth and reorganization phases (G1 and G2) separate the S and
M phase. Cells can enter the G0
phase, or phase of quiescence where they
stop cycling after division.3
Two types of cell cycle control mechanisms regulate the cell cycle. One is a
cascade of protein phosphorylation events that relay a cell from one stage to
the next. Protein phosphorylation involves protein kinases, which associate
with a second subunit (cyclin) that is transiently expressed at the appropriate
period of the cell cycle. The cyclin subunit associates with a cyclin-dependent
kinase (CDK) to create an active complex. Regulatory phosphorylation and
dephosphorylation controls the CDK-cyclin complex. The cyclins and CDKcyclin complexes phosphorylate healthy proteins and move them into the
next phase.3
CDKs 1-6 associate with the cell cycle phases, while CDKs 7-11
regulate RNA transcription.4 Growth signals trigger the growth phase and
retinoblastoma (Rb) protein phosphorylation. The Ink4 family induces G1
phase arrest and inhibits CDK4 or CDK6 or the Cip/Kip family, suppressing
CDK2 activity.2
Cell proliferation
DRIVERS OF TUMORIGENESIS AND TUMOR GROWTH
The second cell cycle control mechanism is a set of checkpoints that monitor
event completion and delay progression to the next stage if necessary.
Specific checkpoints detect mistakes in DNA replication and chromosome
segregation and signal a delay in cycle progression until the mutation danger
has passed.3
Cancer cells ignore all regulatory signals and freely circulate through the cell
division cycle, even in the absence of growth signals due to mutations present
in the regulatory genes. Normally, RB phosphorylation is triggered by growth
signals, but in some cancer cells, pRB brakes are defective, which results in
E2F-dependent G1-S expression. Other common mutations present in cancer
cell genes often include those found in mitogenic signaling pathways like
HER2/ErbB2/Neu receptors, and downstream signaling pathways like RasRaf-MAPK or PI3K-Akt. In addition, the cell cycle-regulation genes/proteins
such as cyclin and CDK proteins are often dysregulated in cancer cells.4,2
In normal cells, specific cell cycle checkpoints detect DNA damage, which
is then repaired by the DNA damage response. The DNA damage response
includes lesion detection, temporary cell cycle arrest, and DNA damage
repair.5
The cell cycle checkpoints allow for the cell cycle machinery to
coordinate biochemical pathways that respond to damaged DNA. Checkpoint
control mechanisms arrest the cell replication phases of the cell cycle and
allow for DNA damage repair. Loss of these checkpoints and failure of
DNA repair due to mutations in the cell cycle machinery can lead to cancer
phenotypes.6
Oncology Guide - Cellular signaling processes involved in cancer development and progression
6 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Contents of Cell Biology for Seminars | Learn Science at Scitable. Accessed May 24, 2022. https://www.
nature.com/scitable/ebooks/cell-biology-for-seminars-14760004/122995941/
2. Williams GH, Stoeber K. The cell cycle and cancer. The Journal of Pathology. 2012;226(2):352-364.
doi:10.1002/path.3022
3. Collins K, Jacks T, Pavletich NP. The cell cycle and cancer. Proceedings of the National Academy of Sciences.
1997;94(7):2776-2778. doi:10.1073/pnas.94.7.2776
4. Ding L, Cao J, Lin W, et al. The Roles of Cyclin-Dependent Kinases in Cell-Cycle Progression and Therapeutic
Strategies in Human Breast Cancer. International Journal of Molecular Sciences. 2020;21(6):1960.
doi:10.3390/ijms21061960
5. Campos A, Clemente-Blanco A. Cell Cycle and DNA Repair Regulation in the Damage Response: Protein
Phosphatases Take Over the Reins. Int J Mol Sci. 2020;21(2):446. doi:10.3390/ijms21020446
6. Solier S, Zhang YW, Ballestrero A, Pommier Y, Zoppoli G. DNA Damage Response Pathways and Cell Cycle
Checkpoints in Colorectal Cancer: Current Concepts and Future Perspectives for Targeted Treatment. Curr
Cancer Drug Targets. 2012;12(4):356-371. doi:10.2174/156800912800190901
7. Alhmoud JF, Woolley JF, Al Moustafa AE, Malki MI. DNA Damage/Repair Management in Cancers. Cancers
(Basel). 2020;12(4):1050. doi:10.3390/cancers12041050
8. Yao Y, Dai W. Genomic Instability and Cancer. J Carcinog Mutagen. 2014;5:1000165. doi:10.4172/2157-
2518.1000165
Cancer can develop as a result of defective DNA repair machinery. The DNA
repair machinery mends genome modifications that occur as a result of
deletions, translocations, loss of heterozygosity, and amplifications in the
DNA. After DNA damage and depending on the type of damage, the following
DNA repair pathways are recruited: nucleotide excision repair, base excision
repair, mismatch repair, or DNA double strand break repair. Defects in any
of these repair genes and pathways cause mutations to accumulate. For
example, ineffective topoisomerase I and topoisomerase II promote DNA
aberrations during replication where DNA strands break. As the mutation
frequency increases, the amount of DNA damage increases and DNA repair
enzymes decrease.7
Thus, any loss in the DNA repair genes leads to genomic
instability and drives tumor development.8
M
G1
G2
S
HER2
Cytoplasm
Nucleus
DNA
RNA Processing
Mitogenic
signals
Dysregulation of
the cell cycle
Cell survival
and proliferation
PI3K
Akt
RAS
RAF
MEK
ERK
RB
RB
E2F
E2F
RB
mTOR
CDK2
Cyclin A/E
CDK8/19
Cyclin C
CDK7
Cyclin H
CDK9
Cyclin T
CDK11
Cyclin L
CDK4/6
Cyclin D
CDK4/6
Cyclin D
CDK2
Cyclin E
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
7 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
M
G1
G2
S
HER2
Cytoplasm
Nucleus
DNA
RNA Processing
Mitogenic
signals
Dysregulation of
the cell cycle
Cell survival
and proliferation
PI3K
Akt
RAS
RAF
MEK
ERK
RB
RB
E2F
E2F
RB
mTOR
CDK2
Cyclin A/E
CDK8/19
Cyclin C
CDK7
Cyclin H
CDK9
Cyclin T
CDK11
Cyclin L
CDK4/6
Cyclin D
CDK4/6
Cyclin D
CDK2
Cyclin E
Oncology Guide - Cellular signaling processes involved in cancer development and progression
8 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
A balance between cell survival and death is crucial for multicellular organism
survival. Organisms must eliminate damaged or infected cells to avoid
interference with normal functions. Imbalances in this process can lead to
uncontrolled cell growth and cancer development.
Apoptosis is a genetically programmed mechanism that results in cell death
and removal of damaged cells. An anti-apoptotic cell phenotype is a hallmark
characteristic for cells to become cancerous.1
Apoptotic pathways are
activated by death receptors on the cell surface, growth factor signal loss, or
in response to lethal stimuli from inside the cell.2
Apoptotic pathways are extrinsic or intrinsic. The TP53 gene encodes p53,
a tumor suppressor that activates both the extrinsic and intrinsic apoptotic
pathways.3
A sub-group of Tumor Necrosis Factor (TNF) receptors that
include TNFR, Fas, and TRAIL mediate the extrinsic pathway. Activation of
these receptors allows for recruitment and activation of caspases 8 and
10, which then forms and activates complexes such as the death inducing
signaling complex (DISC). The complex then activates the effector caspase,
caspase 3, which cleaves the death substrates that lead to apoptosis.1
Upon ligand binding to the Fas receptor, FADD is recruited and caspase 8 is
activated, triggering apoptosis execution. The FLIP protein inhibits FADD by
binding to it and rendering it ineffective.4
The intrinsic pathway involves the
mitochondria and is initiated by stress. Upon stress initiation, the proteins of
the Bcl-2 family, Bax and Bak, are activated and initiate cytochrome c release
from the mitochondria. Cytochrome c release activates caspase 3, which then
leads to apoptosis. Other pro-apoptotic proteins released by the mitochondria
include Smac/Diablo (Second Mitochondrial derived activator of Caspase/
Direct IAP- Binding protein with a low pI) and the serine protease Omi/HtrA2.1
Cell survival
DRIVERS OF TUMORIGENESIS AND TUMOR GROWTH
The PI3K/AKT pathway is indicated in tumor development and progression.5
Mutations that occur in oncogenes and tumor suppressor genes lead to the
dysregulation of the PI3K/AKT pathway, which promotes AKT interference
with cell death signaling pathways. Receptor tyrosine kinases (RTK) are
activated upon binding of epidermal growth factor I (EFG), fibroblast growth
factor receptor (FGF), and insulin-like growth factor (IGF) to its N-terminal
extracellular domain.6
Upon binding of a ligand to RTK, tyrosine kinase
phosphorylation is triggered and activates PI3K. Activated PI3K recruits AKT
by phosphorylating the protein. Activated AKT inactivates proteins like Bax
and Bad. AKT also activates NF-kB, resulting in transcription of pro-survival
genes like Bcl-XL (B-cell lymphoma-extra-large).5
Evidence suggests that cancer also involves mechanisms of apoptosis
resistance and that some cancers result from the lack of cell death. The
p53 protein is commonly mutated in human cancers, which disturbs the
levels of apoptosis regulation. In addition, the Fas receptor is downregulated
in hepatomas. Further, altered TNF family receptors are identified in some
cancers and FLIP is overexpressed in carcinomas. Bcl-2 is overexpressed in a
variety of cancers, including multiple myeloma, acute lymphocytic leukemia,
and chronic lymphocytic leukemia. Thus, pro-apoptotic receptors in cancer
are targets of some therapies.5
Autophagy is another important cellular degradation pathway essential
to cellular homeostasis. While apoptosis prevents cancer cell survival,
autophagy removes oncogenic molecules and prevents cancer cell
survival. Autophagy is divided into 5 stages: initiation, autophagosome
nucleation, autophagosome membrane expansion and elongation, closure
and fusion with the lysosome, and intravesicular product degradation.
Oncology Guide - Cellular signaling processes involved in cancer development and progression
9 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Initiation involves inactivation of mTOR in response to autophagy signals.
PI3K/AKT/mTOR signaling controls autophagy, since mTOR activation
inhibits the process. Subsequently, the Unc-51-like kinase 1 (ULK-1) complex
is activated. This complex stimulates autophagosome nucleation by
activating the class III P13K complex. This induces phagophore formation
through production of PI3P and association with WIPI protein family
members. During elongation, ATG12-ATG5-ATG16L1 and ATG4B-ATG7-ATG3
work together to activate LC3 into LC3I, lipidation with PE to form LC3II, and
anchoring to the phagophore. LC3 and GABARAP mediate the collection of
autophagic substrates before closure. Fusion of the lysosome occurs through
the interaction between STX17 and VAMP8. During intravesicular product
degradation, acidic lysosomal hydrolases degrade the substrates collected,
generating nutrients that are then released to the cytoplasm and reused
by the cell. Evidence suggests that autophagy and apoptosis are closely
interconnected, since some proteins have dual roles in both processes.
Autophagy facilitates apoptosis by degrading a negative regulator of Fas and
modifies levels of Bcl-2. 7,8 Moreover, autophagy can be tumor-promoting or
tumor-inhibiting. Tumors are exposed to stressful conditions and autophagy
acts as a regulator of tumor promotion by helping them overcome these
stresses. The process supplies nutrients to meet the metabolic demands
of tumors, thus increasing cell survival, tumor growth, and oncogenesis.
Autophagy is also a regulator of tumor suppression by offering protective
effects for the cell and reducing the amount of damaged cellular parts and
proteins, which maintains cellular homeostasis. Thus, an impaired autophagy
process can lead to oncogenesis.9
References
1. Portt L, Norman G, Clapp C, Greenwood M, Greenwood MT. Anti-apoptosis and cell survival: A review.
Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 2011;1813(1):238-259. doi:10.1016/j.
bbamcr.2010.10.010
2. Burz C, Berindan-Neagoe I, Balacescu O, Irimie A. Apoptosis in cancer: Key molecular signaling pathways and
therapy targets. Acta Oncologica. 2009;48(6):811-821. doi:10.1080/02841860902974175
3. Su M, Mei Y, Sinha S. Role of the Crosstalk between Autophagy and Apoptosis in Cancer. J Oncol.
2013;2013:102735. doi:10.1155/2013/102735
4. Elmore S. Apoptosis: A Review of Programmed Cell Death. Toxicol Pathol. 2007;35(4):495-516.
doi:10.1080/01926230701320337
5. Kalimuthu S, Se-Kwon K. Cell Survival and Apoptosis Signaling as Therapeutic Target for Cancer: Marine
Bioactive Compounds. Int J Mol Sci. 2013;14(2):2334-2354. doi:10.3390/ijms14022334
6. Rascio F, Spadaccino F, Rocchetti MT, et al. The Pathogenic Role of PI3K/AKT Pathway in Cancer Onset and
Drug Resistance: An Updated Review. Cancers (Basel). 2021;13(16):3949. doi:10.3390/cancers13163949
7. Mulcahy Levy JM, Thorburn A. Autophagy in cancer: moving from understanding mechanism to improving
therapy responses in patients. Cell Death Differ. 2020;27(3):843-857. doi:10.1038/s41418-019-0474-7
8. Alvarez-Meythaler JG, Garcia-Mayea Y, Mir C, Kondoh H, LLeonart ME. Autophagy Takes Center Stage as a
Possible Cancer Hallmark. Frontiers in Oncology. 2020;10. Accessed July 13, 2022. https://www.frontiersin.
org/articles/10.3389/fonc.2020.58606
9. Yun CW, Lee SH. The Roles of Autophagy in Cancer. Int J Mol Sci. 2018;19(11):3466. doi:10.3390/
ijms19113466
Nucleus
Mitochondria Cytoplasm
Anti-apoptotic
genes (Bcl-XL)
Apoptosis
Cytochrome C
Caspase 3
Caspase 8
Bad
Bax/Bak
Stimuli (DNA damage, irradiation, etc.)
PI3K
Akt
FADD
FLIP
NFκB
NFκB
Complex 1
Complex 2
(DISC)
Fas TRAIL TNF RTK
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
10 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Nucleus
Mitochondria Cytoplasm
Anti-apoptotic
genes (Bcl-XL)
Apoptosis
Cytochrome C
Caspase 3
Caspase 8
Bad
Bax/Bak
Stimuli (DNA damage, irradiation, etc.)
PI3K
Akt
FADD
FLIP
NFκB
NFκB
Complex 1
Complex 2
(DISC)
Fas TRAIL TNF RTK
Oncology Guide - Cellular signaling processes involved in cancer development and progression
11 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Cancer cells alter metabolism to promote growth, survival, proliferation, and
long-term maintenance by increasing glucose uptake and fermenting glucose
to lactate. Glucose metabolism is essential for cells to generate energy. In
a normal cell with optimal oxygen levels, full glucose oxidation occurs via
respiration in the mitochondria. Glycolysis converts glucose into pyruvate
that enters the mitochondria where it is oxidized by the citric acid cycle
to generate ATP and CO2
. Tumors and other actively dividing cells switch
from oxidative phosphorylation to aerobic glycolysis where glucose uptake
increases and lactate is produced, even in the presence of oxygen and a
functioning mitochondria. This process is also known as the Warburg Effect.1
Pathways such as phosphoinositide 3-kinase/protein kinase B/mammalian
target of rapamycin (PI3K/Akt/mTOR) and hypoxia-inducible factor-1 (HIF-1)
are glycolysis regulators.2
The Warburg Effect results from HIF-1 upregulation,
oncogene (cMyc, Ras) activation, tumor suppressor (mutant-p53, mutantphosphatase and tensin homolog deleted from chromosome 10 [PTEN]) loss
of function, or P13K/Akt/mTOR activation.3
The P13K/Akt/mTOR pathway is commonly activated in cancers in response
to glucose metabolism. When activated, receptor tyrosine kinases (RTK)
lead to phosphorylation of the binding sites that recruit PI3K and Ras to the
plasma membrane. Upon activation of PI3K, Akt is recruited and activated.
mTOR is then activated and stimulates growth-related protein Myc translation
and increases HIF transcriptional activity. Normally, the tumor suppressor
p53 regulates PTEN, which down-regulates the PI3K pathway. Mutations in
these genes in cancer cells cause loss-of-function. p53 also down-regulates
glycolysis and enhances mitochondrial oxidative phosphorylation in normal
cells. Loss of these tumor suppressors in cancer cells results in activating
growth-promoting mechanisms.4
DRIVERS OF TUMORIGENESIS AND TUMOR GROWTH
Metabolism
Key processes required for the Warburg effect are modulated by HIF-1
activation.4
The expression of glucose transporters and activation of
glycolytic enzymes are enhanced by HIF-1. HIF-1 also prevents the citric
acid cycle and oxidative phosphorylation process by activating pyruvate
dehydrogenase kinase 1 (PDK1), which prevents pyruvate dehydrogenase
(PDH) from converting pyruvate into acetyl-CoA and limits entry of pyruvate
into the citric acid cycle. Additionally, HIF-1 activates max interactor 1 (MXI 1)
and cytochrome c oxidase subunit 4 (COX4). This results in a decrease in
mitochondrial activities and oxygen consumption. Finally, HIF-1 stimulates
lactate dehydrogenase (LDHA) expression, which results in an increase in
lactate production.5
Additional lactate produced as a result of the Warburg effect reduces pH
levels and creates an acidic microenvironment. This microenvironment
can enhance tumor invasion and metastasis, while also increasing ionizing
radiation resistance. Thus, the Warburg effect is another method in which
cancer cells use cellular stress to progress.6
Oncology Guide - Cellular signaling processes involved in cancer development and progression
12 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Liberti MV, Locasale JW. The Warburg Effect: How Does it Benefit Cancer Cells? Trends Biochem Sci.
2016;41(3):211-218. doi:10.1016/j.tibs.2015.12.001
2. Courtnay R, Ngo DC, Malik N, Ververis K, Tortorella SM, Karagiannis TC. Cancer metabolism and the Warburg
effect: the role of HIF-1 and PI3K. Mol Biol Rep. 2015;42(4):841-851. doi:10.1007/s11033-015-3858-x
3. Sharma A, Sinha S, Shrivastava N. Therapeutic Targeting Hypoxia-Inducible Factor (HIF-1) in Cancer: Cutting
Gordian Knot of Cancer Cell Metabolism. Frontiers in Genetics. 2022;13. Accessed June 30, 2022. https://
www.frontiersin.org/article/10.3389/fgene.2022.849040
4. Cairns R, Harris I, McCracken S, Mak T. Cancer Cell Metabolism. Cold Spring Harbor symposia on quantitative
biology. 2011;76:299-311. doi:10.1101/sqb.2011.76.012856
5. Zhao L, Mao Y, Zhao Y, Cao Y, Chen X. Role of multifaceted regulators in cancer glucose metabolism and their
clinical significance. Oncotarget. 2016;7:31572-31585. doi:10.18632/oncotarget.7765
6. Mirzaei H, Hamblin MR. Regulation of Glycolysis by Non-coding RNAs in Cancer: Switching on the Warburg
Effect. Molecular Therapy - Oncolytics. 2020;19:218-239. doi:10.1016/j.omto.2020.10.003
RAS
p53 pTEN
p53
PDK1
PI3K
Akt
mTOR
Mitochondria
RTK
Glycolysis Glucose
CO2
Cytoplasm
HIF
LDHA
MYC
PDH
COX4
MXI1
HIF
Glucose
Pyruvate
Lactate
Citric Acid Cycle
Acetyl CoA
Glucose
Transporter
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
13 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
RAS
p53 pTEN
p53
PDK1
PI3K
Akt
mTOR
Mitochondria
RTK
Glycolysis Glucose
CO2
Cytoplasm
HIF
LDHA
MYC
PDH
COX4
MXI1
HIF
Glucose
Pyruvate
Lactate
Citric Acid Cycle
Acetyl CoA
Glucose
Transporter
Oncology Guide - Cellular signaling processes involved in cancer development and progression
14 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Stem cells have the ability to self-renew or maintain a stem cell population
and differentiate into specialized cells, depending on responses to signals.
A normal cell has the ability to maintain a balance between self-renewal and
differentiation. Cellular differentiation involves alterations in gene expression
that depend on chromatin changes, which are accomplished with chromatinremodeling enzymes. These enzymes regulate differentiation through celltype-specific and gene-specific roles. Chromatin-remodeling enzymes either
use ATP hydrolysis to change DNA contacts or covalently modify histone
proteins. ATP-dependent chromatin-remodeling enzymes regulate the balance
between proliferation and differentiation. Chromatin remodeling is linked
to other cellular processes during differentiation, recombination, genome
organization, and the cell cycle.1,2
ATP-dependent chromatin-remodeling enzymes are a part of the SNF2 family
of DNA-dependent ATPases. The classes of ATP-dependent chromatinremodeling enzymes include the SWI/SNF, imitation SWI (ISWI), and
chromodomain and helicase-like domain (CHD) families. The SWI/SNF
protein complexes can include either the ATPase brahma (BRM)- or brahmalike 1 (BRG1)-containing enzyme, which binds to the bromodomain. The
complex binds to acetylated (Ac) histones. The SWI/SNF complex is involved
in embryonic and extraembryonic lineage segregation during preimplantation
development. During this stage, the SWI/SNF-BRG1 complex maintains
chromatin accessibility at STAT-3 binding targets by preventing PcG-mediated
expression.1
This enhances leukemia inhibitory factor (LIF) signaling, which
is involved in cell differentiation. LIF binding to its receptor activates Janus
kinases (JAKs), phosphorylating receptor docking sites and recruiting
proteins like signal transducer and activator of transcription 3 (STAT3).3
LIF
binding initiates the transcription of differentiation, self-renewal, and survival
genes.1
The SWI/SNF complex also prevents Polycomb complex (PRC2), a
transcription repressor, from binding. This allows for transcription to occur.4
DRIVERS OF TUMORIGENESIS AND TUMOR GROWTH
Cell differentiation
Approximately 25% of all cancers have mutations in one or more of the genes
encoding the SWI/SNF chromatin-remodeling complexes. At least 9 different
genes encoding the SWI/SNF subunits can be mutated in cancer.5
Many
gene mutations in the SWI/SNF complex are loss-of-function mutations.
Inactivating SWI/SNF subunits through mutations or deletions cause
defective complex assembly and failure to oppose PRC1/2, resulting in an
imbalance between differentiation and self-renewal. This imbalance impairs
differentiation and allows expansion of progenitor cells and tumorigenesis.6
Mutation of a gene encoding SWI/SNF complex subunit components allows
for the formation of a residual complex that is dependent on other subunits
and necessary for cancer growth.7
The SWI/SNF complex is also involved
in cell cycle regulation and cellular invasion in vivo.8
As discussed in the cell
proliferation section, the cell cycle is disrupted in some cancers. Thus, SWI/
SNF regulation is also affected in these cases.
Chromatin remodelers make DNA accessible for transcription factors and
basal transcription machinery. The SWI/SNF complex remodels chromatin
so genes can be activated or repressed, depending on the interaction
between a variety of transcription factors and other chromatin modifiers. It is
essential for maintaining correct nucleosome positions and any alterations
or disruptions in SWI/SNF function can result in incorrect transcription factor
binding, leading to atypical gene expression patterns. Thus, mutations in
or inactivation of chromatin remodelers can lead to an imbalance between
self-renewal and differentiation, leading to expansion of progenitor cells and
tumorigenesis.2,6
Oncology Guide - Cellular signaling processes involved in cancer development and progression
15 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Hota SK, Bruneau BG. ATP-dependent chromatin remodeling during mammalian development. Development.
2016;143(16):2882-2897. doi:10.1242/dev.128892
2. Skulte KA, Phan L, Clark SJ, Taberlay PC. Chromatin remodeler mutations in human cancers: epigenetic
implications. Epigenomics. 2014;6(4):397-414. doi:10.2217/epi.14.37
3. Morris R, Kershaw NJ, Babon JJ. The molecular details of cytokine signaling via the JAK/STAT pathway.
Protein Sci. 2018;27(12):1984-2009. doi:10.1002/pro.3519
4. Chen T, Dent SYR. Chromatin modifiers: regulators of cellular differentiation. Nat Rev Genet.
2014;15(2):93- 106. doi:10.1038/nrg3607
5. Mittal P, Roberts CWM. The SWI/SNF complex in cancer — biology, biomarkers and therapy. Nat Rev Clin
Oncol. 2020;17(7):435-448. doi:10.1038/s41571-020-0357-3
6. Lu C, Allis CD. SWI/SNF Complex in Cancer: ‘Remodeling’ Mechanisms Uncovered. Nat Genet.
2017;49(2):178- 179. doi:10.1038/ng.3779
7. Helming KC, Wang X, Roberts CWM. Vulnerabilities of Mutant SWI/SNF Complexes in Cancer. Cancer Cell.
2014;26(3):309-317. doi:10.1016/j.ccr.2014.07.018
8. Smith JJ, Xiao Y, Parsan N, et al. The SWI/SNF chromatin remodeling assemblies BAF and PBAF differentially
regulate cell cycle exit and cellular invasion in vivo. PLOS Genetics. 2022;18(1):e1009981. doi:10.1371/journal.
pgen.1009981
JAK1
STAT3 STAT3
STAT3
JAK1
STAT3
Nucleus
Inactive
Active
Active
Cell
cycle
Cytoplasm
Differentiation genes
LIF
CDK2
Cyclin E M
G1
G2
S
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
PRC2
Click to enlarge
x
Imbalanced Differentiation/Self-renewel
Differentiation Self-renewal
Balanced Differentiation/Self-renewel
Differentiation Self-renewal
Histone
Differentiation gene
expression
Cancer Cell
Nucleus
Gene transcription
inhibited by PRC2
SWI/SNF
complex
SWI/SNF
complex
Mutated
SWI/SNF
complex
Healthy Cell
JAK1
STAT3
JAK1
STAT3
STAT3
Nucleus
Cytoplasm
Extracellular space
PRC2 PRC2
SWI/SNF
complex
JAK1
STAT3
JAK1
STAT3
STAT3
Cytoplasm
Extracellular space
STAT3 PRC2
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
16 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
JAK1
STAT3 STAT3
STAT3
JAK1
STAT3
Nucleus
Inactive
Active
Active
Cell
cycle
Cytoplasm
Differentiation genes
LIF
CDK2
Cyclin E M
G1
G2
S
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
SWI/SNF
Bromo ATPase
PRC2
Oncology Guide - Cellular signaling processes involved in cancer development and progression
17 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
x
Imbalanced Differentiation/Self-renewel
Differentiation Self-renewal
Balanced Differentiation/Self-renewel
Differentiation Self-renewal
Histone
Differentiation gene
expression
Cancer Cell
Nucleus
Gene transcription
inhibited by PRC2
SWI/SNF
complex
SWI/SNF
complex
Mutated
SWI/SNF
complex
Healthy Cell
JAK1
STAT3
JAK1
STAT3
STAT3
Nucleus
Cytoplasm
Extracellular space
PRC2 PRC2
SWI/SNF
complex
JAK1
STAT3
JAK1
STAT3
STAT3
Cytoplasm
Extracellular space
STAT3 PRC2
Oncology Guide - Cellular signaling processes involved in cancer development and progression
18 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
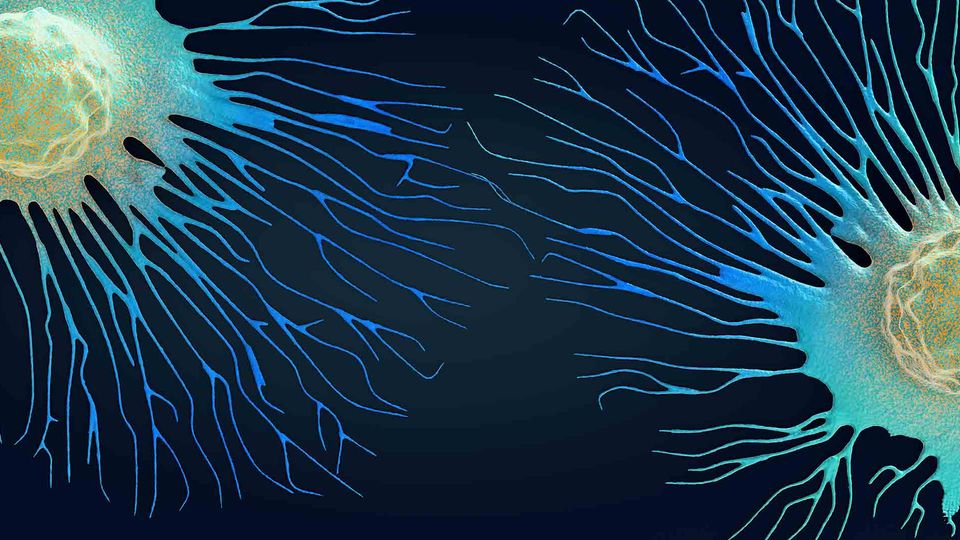
While treating cancer in early stages is the ideal course of therapy and the
reason why preventative care is such a focus of modern medicine, there are
some cancers that progress aggressively and do not present symptoms
until advanced stages. Once a tumor is established, it moves to invade and
metastasize into nearby tissues. As with the early stages of tumor growth,
metastasis requires an assortment of mutations and imbalances. Epithelial
cells transition to the mesenchymal phenotype (EMT), which allows for
higher mobility and cancer cell invasiveness. Overall, loss of cell polarity
is commonly observed in cancer and facilitates invasion and metastasis.
These physical changes enable the cancer cells to readily travel through
blood vessels and target tissues and organs. Paired with the physiological
process of angiogenesis, the tumor is established and able to grow – even
in a hypoxic and nutrient deficient environment. Within this section we have
presented key pathways that drive critical cellular changes that are exhibited
during cancer progression. These processes all represent targets of drug
discovery efforts to slow cancer spread, control patient symptoms, and
prolong life.
TUMOR INVASION & METASTASIS
Introduction
Cancer
cell
Healthy
cell
Adhesion
molecules
ECM
Blood vessel
ECM
Blood vessel
Cancer cell
migration and
invasion
Cytoplasm
Loss of Polarity
Cytoskeletal
changes
Dvl
Wnt Vang Extracellular
space
TCF/
LEF
Dvl
Gene
transcription
Cytoplasm
Wnt
RTK
Increased
motility
Cell migration
Nucleus
Induction of Migration
PI3K RAS
B-catenin
B-catenin
B-catenin
destruction
complex
Cytoplasm
Induction of EMT
Nucleus
Rho Rac
Gene
transcription
EMT
SMAD
2/3
SMAD
2/3
Translational
regulation
Cytoskeletal
changes
Extracellular space Extracellular space
PI3K
SMAD4
TGF-β
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
19 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Cancer
cell
Healthy
cell
Adhesion
molecules
ECM
Blood vessel
ECM
Blood vessel
Cancer cell
migration and
invasion
Cytoplasm
Loss of Polarity
Cytoskeletal
changes
Dvl
Wnt Vang Extracellular
space
TCF/
LEF
Dvl
Gene
transcription
Cytoplasm
Wnt
RTK
Increased
motility
Cell migration
Nucleus
Induction of Migration
PI3K RAS
B-catenin
B-catenin
B-catenin
destruction
complex
Cytoplasm
Induction of EMT
Nucleus
Rho Rac
Gene
transcription
EMT
SMAD
2/3
SMAD
2/3
Translational
regulation
Cytoskeletal
changes
Extracellular space Extracellular space
PI3K
SMAD4
TGFβ
Oncology Guide - Cellular signaling processes involved in cancer development and progression
20 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
In epithelial cells, apical-basal polarity and contact with adjacent cells
occurs through adherens, tight junctions, and desmosomes. In contrast,
mesenchymal cells do not have apical-basal polarity or a basal lamina
separating them from the adjacent tissue and are separated from other cells
by the extracellular matrix. During epithelial-mesenchymal transitions (EMT)
that occur during biological processes and cancer progression, epithelial
cells obtain mesenchymal features. In this process, epithelial cells lose
adherent junction and downregulate cytokeratins and E-cadherin, epithelial
specific markers. They also gain a fibroblastoid invasive phenotype by
increasing mesenchymal markers like fibronectin, N-cadherin, and vimentin.1
Thus, EMT results in changes in epithelial cell polarity from apical-basal to
anteroposterior, transitions from epithelial to mesenchymal phenotype, and
allows for higher mobility and cancer cell invasiveness.2
EMT is regulated by highly conserved molecular steps. Cancer cells that
undergo EMT secrete cytokines such as TGF-β, which is the primary inducer
of EMT. TGF-β binds the serine/threonine kinase receptors TGF-β receptor
type I (TβRI) and type II (TβRII). Upon activation of these receptors, SMAD
and non-SMAD signaling pathways are activated. Specifically, activated TβRI
phosphorylates SMAD2/3 that is associated with SMAD4. This complex is
transported to the nucleus, where it regulates the transcription of EMT-related
genes. The key transcription factors activated by TGF-β are SNAIL, ZEB, and
TWIST. SNAIL is an inducer of EMT, while TWIST and ZEB keep the invasive
mesenchymal phenotype. TGF-β may induce EMT through non-SMAD
pathways through activation of the PI3K-AKT signaling pathway that leads to
translational regulation of EMT factors. TGF-β can also initiate the Rac/Rho
pathway and initiate cytoskeletal changes.2
TUMOR INVASION & METASTASIS
Epithelial-mesenchymal transition (EMT)
Overall, activation of EMT transcription factors leads to reducing specific
genes that encode for proteins involved in forming adherens and tight
junctions, desmosomes, and maintaining the apical-basal cell polarity. These
junctions support the epithelial phenotype and control various signaling
pathways through associated proteins. Thus, dysregulation of cell-cell
junctions affects molecular pathways and can further activate EMT and
cancer invasion. The mesenchymal phenotype also promotes cell migration,
which increases cancer motility and invasion into neighboring tissues.2
One of
the first steps of metastasis is invasion of cells into the extracellular matrix.
Thus, cells obtaining the ability to migrate and invade is the hallmark of EMT
and describes the role of EMT in metastasis.1
Oncology Guide - Cellular signaling processes involved in cancer development and progression
21 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Ribatti D, Tamma R, Annese T. Epithelial-Mesenchymal Transition in Cancer: A Historical Overview. Transl
Oncol. 2020;13(6):100773. doi:10.1016/j.tranon.2020.100773
2. Škovierová H, Okajčeková T, Strnádel J, Vidomanová E, Halašová E. Molecular regulation of epithelial-tomesenchymal transition in tumorigenesis (Review). Int J Mol Med. 2018;41(3):1187-1200. doi:10.3892/
ijmm.2017.3320
Akt
RhoA SMAD2
SMAD3
SMAD2
SMAD4
SMAD3
Rac PI3K
Nucleus
Cytoplasm TβRI TβRII
Mesenchymal gene activation,
epithelial gene repression
EMT gene expression
Cytoskeletal changes
Translational regulation
TGF-β
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
22 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Akt
RhoA SMAD2
SMAD3
SMAD2
SMAD4
SMAD3
Rac PI3K
Nucleus
Cytoplasm TβRI TβRII
Mesenchymal gene activation,
epithelial gene repression
EMT gene expression
Cytoskeletal changes
Translational regulation
TGF-β
Oncology Guide - Cellular signaling processes involved in cancer development and progression
23 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Cell polarity is essential for maintaining cellular homeostasis and organizing
intracellular pathways. Cell migration and invasion involve changes in cell
shape, which requires the loss of apical-basal polarity and organizing frontrear polarity. The process is tightly controlled in normal cells, since excess
cell migration can result in serious pathological consequences.1
Cellular
architecture is organized along the apical-basal axis that is associated with
epithelial signaling and the planar axis orthogonal to the apical-basal axis that
organizes cell polarity.2
Loss of cell polarity is commonly observed in cancer
and facilitates invasion and metastasis.1
Three complexes establish and preserve apical-basal polarity: the Par,
Scribble, and Crumbs complexes. The Par complex is located at the apical
side within tight junctions and promotes formation and maintenance of these
areas. It consists of Par3, Par6, and aPKC (apical protein kinase C). Par3 and
Par6 mediate protein-protein interactions and associate with tight junction
proteins and aPKC. The Rho GTPases Rac1 and Cdc42 associate with the
Par complex and activate aPKC. This then phosphorylates Crumbs, Lgl, and
GSK3β (glycogen synthase kinase-3β). The Crumbs complex also localizes to
the apical side and consists of Pals1 and PATJ. PATJ promotes tight junction
formation. The Scribble complex localizes basolaterally and comprises
Scribble, Dlg, and Lgl. aPKC regulates signaling events for establishing apicalbasal, front-rear polarity, and cell invasion.1
Planar cell polarity (PCP) proteins generate polarity orthogonal to the
apical-basal axis and coordinate cell division and cilia function. Planar cell
polarity proteins include Van Gogh (Vang), Frizzled (Fz), Dishevelled (Dvl),
and the signaling ligand Wnt, which localize to the cytoplasm. Regulation of
these components leads to cell migration and invasion that occurs through
the asymmetrical localization of the PCP proteins and migration of cells
orthogonal to apicobasal polarity.1
Increasing evidence shows that the Wnt/
TUMOR INVASION & METASTASIS
Cell polarity
PCP signaling pathway promotes the proliferative and migratory properties of
tumor cells. Wnt/PCP signaling is adapted to promote cancer cell migration,
since it results in the mutual antagonism between Fzd/Dvl and Vang/Pk
complexes, leading to cytoskeletal rearrangements. The expression of core
PCP components is elevated in some cancers.2
Destabilization of junctional complexes and loss of epithelial polarity is
commonly associated with cancer. Invasive cancer cells use the epithelialmesenchymal transition to develop from the mesenchymal mode. During
this process, the polarity complexes are deconstructed and loss of the
epithelial cell-cell junctions and apical-basal polarity occurs, which establishes
a front-rear polarity. Proto-oncogenes such as Ras and PI3K/AKT activate
the epithelial-mesenchymal transition, which increases the invasive and
metastatic potential of cancer cells.1,3
Oncology Guide - Cellular signaling processes involved in cancer development and progression
24 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Gandalovičová A, Vomastek T, Rosel D, Brábek J. Cell polarity signaling in the plasticity of cancer cell
invasiveness. Oncotarget. 2016;7(18):25022-25049. doi:10.18632/oncotarget.7214
2. VanderVorst K, Hatakeyama J, Berg A, Lee H, Carraway KL. Cellular and Molecular Mechanisms Underlying
Planar Cell Polarity Pathway Contributions to Cancer Malignancy. Semin Cell Dev Biol. 2018;81:78-87.
doi:10.1016/j.semcdb.2017.09.026
3. Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial–mesenchymal transition. Nat Rev Mol Cell
Biol. 2014;15(3):178-196. doi:10.1038/nrm3758
Crumbs
Crumbs PATJ Pals1
Par6
Par6
Par3 Cdc42
Cdc42
Gsk3β
Gsk3β
Rac1
aPKC aPKC
aPKC
Lgl
Lgl
Lgl Scribble
Dlg
Basal Membrane
T
J
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
25 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Crumbs
Crumbs PATJ Pals1
Par6
Par6
Par3
Cdc42
Cdc42
Gsk3β
Gsk3β
Rac1
aPKC
aPKC
aPKC
Lgl
Lgl
Lgl Scribble
Dlg
Basal Membrane
TJ
Oncology Guide - Cellular signaling processes involved in cancer development and progression
26 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Increased cell migration is a factor in cancer development and metastasis.
Genetic and epigenetic changes and dysregulation in cell migration signaling
pathways cause carcinogenesis.1
Metastasis development from a primary
tumor site is a multistep event and includes epithelial-mesenchymal
transition (EMT), tumor neoangiogenesis, and spread of malignancy. Spread
of malignancy occurs from malignant cell transport through blood vessels,
targeting tissues and organs.2
Developmental pathways such as Wnt and receptor tyrosine kinase (RTK)
control cell migration and are commonly overactivated in solid tumors and
metastasis. Wnt signaling molecules bind to the frizzled family of receptors
and is either canonical (β-catenin dependent) or non-canonical (β-catenin
independent). The canonical pathway is activated upon binding to a ligand.
Wnt triggers a signaling cascade that results in cell migratory gene activation.
Wnt binding to frizzled-7 leads to recruitment of Dishevelled (Dvl) proteins,
which promotes β-catenin destruction complex disaggregation. The complex
is composed of the tumor suppressor adenomatous polyposis coli (APC),
the serine/threonine protein kinase glycogen synthase kinase 3 (GSK3), Axin,
and casein kinase (CKI). The disaggregation of the β-catenin destruction
complex inactivates it and results in β-catenin accumulation in the cytoplasm.
β-catenin then migrates to the nucleus and interacts with the TCF/LEF-1
family of transcription factors. These transcription factors activate genes
encoding for proteins involved in EMT and motility (Snail).2,3
TUMOR INVASION & METASTASIS
Cell migration
RTKs are cell surface receptors that mediate signaling pathways
involved in cell migration and are often mutated in a variety of cancers.
Mutations that affect RTKs result in increased cell migration. RTKs are
auto-phosphorylated upon ligand binding, which activates Ras and induces
Raf. Raf phosphorylates MEK, which phosphorylates ERK. Raf also activates
the MAP3 kinase signaling cascade that activates MKK, MEK, and ERK. RTK
auto-phosphorylation also activates the PI3K pathway, which activates Akt
and induces mTOR.4
During metastasis, which occurs in late stage cancer, tumors may
undergo EMT by which polarized epithelial cells transform into migratory
mesenchymal cells with invasive properties. Activation of Wnt signaling
stabilizes transcriptional factors that are responsible for EMT. In addition,
pharmacological inhibition of the PI3K-Akt signaling pathway in cells
with hyperactivated Wnt signaling leads to β-catenin accumulation in the
nucleus, resulting in increased metastasis. Further, exosomes are vehicles
for transporting active Wnt ligands or incorporating β-catenin and may be a
mechanism in which tumors prime their metastatic niche.5
Oncology Guide - Cellular signaling processes involved in cancer development and progression
27 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Derakhshani A, Rostami Z, Safarpour H, et al. From Oncogenic Signaling Pathways to Single-Cell Sequencing
of Immune Cells: Changing the Landscape of Cancer Immunotherapy. Molecules. 2021;26(8):2278.
doi:10.3390/molecules26082278
2. Nwabo Kamdje AH, Takam Kamga P, Tagne Simo R, et al. Developmental pathways associated with cancer
metastasis: Notch, Wnt, and Hedgehog. Cancer Biol Med. 2017;14(2):109-120. doi:10.20892/j.issn.2095-
3941.2016.0032
3. Sedgwick AE, D’Souza-Schorey C. Wnt Signaling in Cell Motility and Invasion: Drawing Parallels between
Development and Cancer. Cancers (Basel). 2016;8(9):80. doi:10.3390/cancers8090080
4. Regad T. Targeting RTK Signaling Pathways in Cancer. Cancers (Basel). 2015;7(3):1758-1784. doi:10.3390/
cancers7030860
5. Zhan T, Rindtorff N, Boutros M. Wnt signaling in cancer. Oncogene. 2017;36(11):1461-1473. doi:10.1038/
onc.2016.304
PI3K
Akt
RAS
RAF
MKK MEK
mTOR
MAP3K
Nucleus
Cytoplasm
RTK Frizzled
Dvl
Cell migration
Increased motility,
metastasis
Wnt
Axin CKl
GSK
β-catenin
β-catenin
β-catenin
β-catenin
APC
TCF/LEF
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
28 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
PI3K
Akt
RAS
RAF
MKK MEK
mTOR
MAP3K
Nucleus
Cytoplasm
RTK Frizzled
Dvl
Cell migration
Increased motility,
metastasis
Wnt
Axin CKl
GSK
β-catenin
β-catenin
β-catenin
β-catenin
APC
TCF/LEF
Oncology Guide - Cellular signaling processes involved in cancer development and progression
29 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Angiogenesis is a physiological process that involves the proliferation,
migration, and morphogenesis of endothelial cells from existing vessels
into new blood vessels. It is a hallmark of cancer and linked to metastasis.
There are several differences between normal angiogenesis and tumor
angiogenesis. One difference involves the source of the endothelial cell
mitogen or chemoattractant. Indeed, tumor cells require invasion of the
epithelial basement membrane to access the blood vessels since they
originate in non-vascularized epithelium. In addition, tumor angiogenesis is
continuous as long as the tumor is in place, whereas normal angiogenesis
continues for a limited amount of time.1
Angiogenesis is triggered by extracellular signals like hypoxia or growth
factors. Tumor cells become hypoxic as they expand away from the blood
supply.1
Angiogenesis allows tumor cells to continue growing, even in a
hypoxic and nutrient deficient environment. The primary driver of this activity
is hypoxia-inducible factor (HIF).2
HIFs are continuously expressed and
degraded under normoxia. Hypoxia is a common characteristic in many types
of solid tumors. Elevated HIF levels are correlated with tumor metastasis,
angiogenesis, poor patient progression as well as tumor resistance to
therapy. Hypoxia, via HIF, upregulates angiogenic growth factors like vascular
endothelial growth factors (VEGF). VEGF and HIF are important signaling
proteins that attract the endothelial cell to the tumor mass and stimulate new
blood vessels or induce growth of pre-existing blood vessels.1
VEGF and other
growth factor stimulation through HIF activates PI3K through AKT, which can
also indirectly activate MAPK. PI3K/AKT activation leads to upregulated VEGF
and HIF transcription.3
Thus, the PI3K/AKT and MAPK signaling pathways
regulate angiogenesis by increasing HIF and VEGF expression in response to
growth factors.3,4
TUMOR INVASION & METASTASIS
Angiogenesis
The tumor microenvironment, which is composed of tumor cells, vascular
endothelial cells, and stromal cells, also regulates tumor angiogenesis.
The PI3K/AKT pathway can control the tumor microenvironment by
regulating endothelial migration, proliferation, and survival. Cancer cell and
vascular endothelial cell interaction in the tumor microenvironment affects
angiogenesis. In cancer cells, growth factors activate the PI3K/AKT/mTOR/
HIF axis and induce VEGF. This increases angiogenic response and activates
endothelial cells. Thus, tumor growth, metastasis, and angiogenesis involve
the PI3K signaling pathway.3,5
Oncology Guide - Cellular signaling processes involved in cancer development and progression
30 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Bielenberg DR, Zetter BR. The Contribution of Angiogenesis to the Process of Metastasis. Cancer J.
2015;21(4):267-273. doi:10.1097/PPO.0000000000000138
2. Heer EC de, Jalving M, Harris AL. HIFs, angiogenesis, and metabolism: elusive enemies in breast cancer. J Clin
Invest. 2020;130(10):5074-5087. doi:10.1172/JCI137552
3. Jiang BH, Liu LZ. PI3K/PTEN Signaling in Angiogenesis and Tumorigenesis. Adv Cancer Res. 2009;102:19-65.
doi:10.1016/S0065-230X(09)02002-8
4. Zhang Z, Yao L, Yang J, Wang Z, Du G. PI3K/Akt and HIF‑1 signaling pathway in hypoxia‑ischemia (Review).
Molecular Medicine Reports. 2018;18(4):3547-3554. doi:10.3892/mmr.2018.9375
5. Jiang X, Wang J, Deng X, et al. The role of microenvironment in tumor angiogenesis. Journal of Experimental
& Clinical Cancer Research. 2020;39(1):204. doi:10.1186/s13046-020-01709-5
Click to enlarge
mTOR
AKT MAPK
PI3K Ras
Nucleus
Cytoplasm
Growth factor
Angiogenesis
VEGF, HIF
transcription
Click to enlarge
Cytoplasm
Nucleus
VEGF
Growth factor
Extracellular space
mTOR AKT PI3K
Pro-angiogenic
gene expression,
e.g. VEGF
Ras Raf MAPK
Normoxic
conditions
Blood vessel
Tumor
Hypoxic
conditions
Oncology Guide - Cellular signaling processes involved in cancer development and progression
31 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
mTOR
AKT MAPK
PI3K Ras
Nucleus
Cytoplasm
Growth factor
Angiogenesis
VEGF, HIF
transcription
Oncology Guide - Cellular signaling processes involved in cancer development and progression
32 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Cytoplasm
Nucleus
VEGF
Growth factor
Extracellular space
mTOR AKT PI3K
Pro-angiogenic
gene expression,
e.g. VEGF
Ras Raf MAPK
Normoxic
conditions
Blood vessel
Tumor
Hypoxic
conditions
Oncology Guide - Cellular signaling processes involved in cancer development and progression
33 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Examining the conditions in which a tumor is growing reveals a complex
ecosystem, tailored to facilitate cancer cell survival and evolving in response
to therapeutic intervention. The extracellular matrix (ECM) is a dynamic
structural component of the microenvironment which can modify cellular
behavior and differentiation. The ECM is involved in the larger picture of
the tumor microenvironment (TME) and includes the basement membrane
(BM), endothelial cells, adipose cells, tumor-infiltrating immune cells, cancerassociated fibroblasts (CAFs), immune cells, and signaling molecules that
regulate tumor progression and expansion. The TME influences accessibility
of therapies to reach the tumor and fosters an environment that facilitates
and promotes both drug resistance and tumor persistence. Deconvolution
of the complexity of the tumor stroma is a critical focus of drug discovery
efforts in order to provide improved and personalized treatment options for
patients, leading to better outcomes.
COMPLEXITY OF THE TUMOR STROMA
Introduction
Click to enlarge
MMP2/MMP9
expression
Altered gene
expression
TGF-β IL-6
IGF/HGF/
EGF
Cancer cell
invasion
Cancer cell
invasion
Cancer cell
invasion
Cytoplasm
Extracellular space
Nucleus
JAK2
Raf STAT3
Rho PI3K Ras
MAPK
FAK
ERK
ILK
NFKB
EMT
FAK
ERK
MEK
FN HA OPN OPN
EMT
Cancer
cell
Healthy
cell
Basement membrane
SMAD
2/3
MMPs
Growth factors
Exosome
IL-6
Cancer cell
invasion
ECM
degradation
Blood vessel
Interstitial membrane
CAF
Neutrophil
TAM
Stromal cell
Oncology Guide - Cellular signaling processes involved in cancer development and progression
34 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
MMP2/MMP9
expression
Altered gene
expression
TGFβ IL-6
IGF/HGF/
EGF
Cancer cell
invasion
Cancer cell
invasion
Cancer cell
invasion
Cytoplasm
Extracellular space
Nucleus
JAK2
Raf STAT3
Rho PI3K Ras
MAPK
FAK
ERK
ILK
NFKB
EMT
FAK
ERK
MEK
FN HA OPN OPN
EMT
Cancer
cell
Healthy
cell
Basement membrane
SMAD
2/3
MMPs
Growth factors
Exosome
IL-6
Cancer cell
invasion
ECM
degradation
Blood vessel
Interstitial membrane
CAF
Neutrophil
TAM
Stromal cell
Oncology Guide - Cellular signaling processes involved in cancer development and progression
35 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
The extracellular matrix (ECM) is a highly dynamic structural component of
the tumor microenvironment. It is made up of a network of biochemically
distinct components that include fibrous proteins, glycoproteins,
proteoglycans, and polysaccharides that work together to provide structural
support for cells. The ECM is constantly being remodeled where components
are deposited, degraded, or modified.1
Cellular behavior and differentiation
are controlled by the ECM and when the dynamics are dysregulated, cancer
development may occur.2
Cells create and rearrange ECM components depending on specific tissue
needs. The major components are collagen, proteoglycans, laminin, and
fibronectin, which make up both the basement membrane and interstitial
matrix. Collagen is the basis of ECM architecture and is involved in wound
repair and organ development. It is found in tendons, cartilage, skin, and
the cornea. Fibrillar collagens are made up of several subtypes of collagen
depending on the tissue location, and ECM proteins mediate their formation.
Proteoglycans are the functional modifiers of the ECM and are characterized
as proteins that have glycosaminoglycans covalently bonded to them. They
vary in size and have integral functions in the ECM, like space-filling and
lubrication, binding to growth factors and other ECM proteins, serving as
a molecular bridge between the cell surface and ECM, and directing organ
size and shape. Laminin connects the cell to the ECM through binding of
integrins. They are involved in adhesion, differentiation, migration, phenotype
maintenance, and apoptotic resistance. Fibronectin is the mechanosensitive
connection between the cell and the ECM.2
Normal ECM dynamics maintain a healthy microenvironment by
keeping tumor-prone cells, fibroblasts, eosinophils, macrophages, and
stromal cells contained. The ECM molecules influence biochemical and
biophysical processes in the cell and besides providing structural support,
COMPLEXITY OF THE TUMOR STROMA
Extracellular matrix (ECM)
determine cell functions and phenotypes. To maintain tissue homeostasis
and balance the deposition and degradation of ECM components, cells
sense ECM properties through contact with focal adhesion complexes. This
regulates the expression of ECM components and enzymes based on signals
of the ECM. Any imbalance in the deposition and degradation of the ECM can
lead to cancer. The ECM also influences cell migration, since cells migrate
from regions with lower ECM concentration to higher ECM concentration.2
Changes to ECM components can dysregulate adhesion and migration, since
the different properties of the ECM are connected. Changes in the ECM can
also influence stromal cell behavior and aid in tumor-associated angiogenesis
and inflammation, leading to a tumorigenic microenvironment. Abnormal
ECM dynamics compromise the basement membrane and promote epithelialmesenchymal transition, allowing for invasion by cancer cells. Activated
fibroblasts or cancer-associated fibroblasts (CAFs) from pathological
conditions promote upregulation of LOX activities, which stabilize collagen
assembly and build the ECM. Thickening of collagen fibers allow for cancer
cells to migrate rapidly to areas enriched in collagen. Immune cells are
recruited to the site of invading cancer cells and promote cancer progression.
The dysregulated ECM promotes tumor-associated angiogenesis, which
allows for tumor cell invasion and metastasis to distant sites where cancer
cells leave circulation and invade local tissues.3
Numerous molecular networks and extracellular molecules regulate
cancer cell invasion and metastatic processes. These include ECM
molecules, ECM receptors, and growth factors. ECM molecules are
hyaluronan (HA), fibronectin (FN), and Small Integrin-Binding Ligand
N-linked Glycoprotein (SIBLING). HA makes up the glycosaminoglycan
present in the ECM and promotes cell invasion through binding to the ECM
receptor CD44 and activating the PI3K/AKT and Rho signaling pathways.
Oncology Guide - Cellular signaling processes involved in cancer development and progression
36 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
References
1. Nallanthighal S, Heiserman JP, Cheon DJ. The Role of the Extracellular Matrix in Cancer Stemness. Frontiers in
Cell and Developmental Biology. 2019;7. Accessed July 7, 2022. https://www.frontiersin.org/articles/10.3389/
fcell.2019.00086
2. Walker C, Mojares E, del Río Hernández A. Role of Extracellular Matrix in Development and Cancer
Progression. Int J Mol Sci. 2018;19(10):3028. doi:10.3390/ijms19103028
3. Lu P, Weaver VM, Werb Z. The extracellular matrix: A dynamic niche in cancer progression. Journal of Cell
Biology. 2012;196(4):395-406. doi:10.1083/jcb.201102147
4. Stivarou T, Patsavoudi E. Extracellular Molecules Involved in Cancer Cell Invasion. Cancers. 2015;7:238-265.
doi:10.3390/cancers7010238
FN is a glycoprotein that is a cell-matrix and cell-cell adhesion mediator.
Overexpression of FN is reported in some cancers and involved in cell
invasion and metastasis through binding to integrins and upregulating the
growth factor matrix metalloproteinases (MMPs) MMP-2 and MMP-9 via
the FAK/ILK/ERK/Pi3K/NF-kB pathways. The SIBLING protein osteopontin
(OPN) is a non-structural ECM protein and identified as a biomarker of tumor
metastasis. OPN binds to integrins and CD44 to promote cancer cell invasion.
MMP-9 over-expression is induced through the FAK/MEK/ERK/NF-kB
pathway when OPN binds to integrin.4
PI3K
NFκB MMP2 MMP9
ERK ERK
ILK MEK
FAK PI3K AKT Rho FAK
Nucleus
Cytoplasm
Cancer cell invasion
Cancer cell invasion
CD44 Integrins Integrins CD44
HA FN OPN OPN
Click to enlarge
Oncology Guide - Cellular signaling processes involved in cancer development and progression
37 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
PI3K
NFκB MMP2 MMP9
ERK ERK
ILK MEK
FAK PI3K AKT Rho FAK
Nucleus
Cytoplasm
Cancer cell invasion
Cancer cell invasion
CD44 Integrins Integrins CD44
HA FN OPN OPN
Oncology Guide - Cellular signaling processes involved in cancer development and progression
38 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
The tumor microenvironment (TME) is a complex and evolving entity that
regulates essential tumor survival and promotion functions.1,2 Early in
tumor growth, cancer cells and the various TME components develop a
relationship. This relationship supports cancer cell survival, local invasion,
and metastasis. Tumor development and progression creates a hypoxic and
acidic environment, so the TME creates a program to promote angiogenesis
that restores oxygen and nutrient supply, while removing metabolic waste.2
The TME comprises the extracellular matrix (ECM) and basement membrane
(BM), endothelial cells, adipose cells, tumor-infiltrating immune cells, cancerassociated fibroblasts (CAFs), immune cells, and signaling molecules that
regulate tumor progression.1
CAFs facilitate crosstalk between cancer cells and the TME and are
developed from tissue resident fibroblasts, adipocytes, endothelial cells,
pericytes, stellate cells, and bone marrow-derived mesenchymal stem cells.
Injury to tissues causes fibroblasts to form myofibroblasts, which produce
transforming growth factor-β (TGF-β). When activated, myofibroblasts play
a role in proliferation, contractile properties, secretory phenotypes, and
ECM formation. In the TME, cancer cells and other stroma cells secrete
growth factors like TGF-β, platelet derived growth factor (PGDF), epidermal
growth factor (EGF), hepatocyte growth factor (HGF), insulin-like growth
factor (IGF), and fibroblast growth factor 2 (FGF2). These growth factors
convert fibroblasts into CAFs, which are similar to myofibroblasts. CAFs also
secrete TGF-β, which allows them to control metastasis, since it is required
for epithelial-mesenchymal transition (EMT) and angiogenesis. During
EMT, epithelial cells lose cell polarity and cell-to-cell adhesions and develop
migratory and invasive phenotypes, making it a critical step in metastasis.2
TGF-β is one of the growth factors that induces EMT through different
pathways such as MAPK, PI3K, and SMAD. Because of these pathways,
COMPLEXITY OF THE TUMOR STROMA
Tumor microenvironment
epithelial features are down-regulated and mesenchymal features are
up-regulated. HGF, IGF, and EGF promote EMT through the PI3K/Akt and Ras/
MAPK pathways.3
CAFs also secrete MMP-3, which promotes cancer cell
invasion through the TME by degrading E-cadherin. MMP-3 releases VEGF
to promote angiogenesis. Thus, CAFs promote tumor develop and migration
through the TME.2
Stromal cells are multipotent stem cells found in various adult tissues,
including bone marrow, adipose tissue, liver, and lung. They are also found
in some tumors and influence TME function and development because
cancer cells often recruit stroma cells from nearby endogenous tissue.1,2
The tumor reprograms cancer-associated stroma cells and enhances
the EMT, which promotes angiogenesis and metastasis. They also aid in
metastasis by secreting exosomes that carry proteins, lipids, miRNAs, and
mRNA.1
Thus, stromal cells facilitate angiogenesis, proliferation, invasion, and
metastasis in the TME.2
Immune cells are another critical component of the TME and can
either suppress or promote tumor growth.2
During every step of cancer
development, cancer cells are exposed to immune cells. Exposure to
antigens activates adaptive immunity, which evaluates cancer cell threat.
Adaptive immune cells are T-cells, B-cells, and natural killer (NK) cells.
Tumor progression activates innate immunity and includes macrophages,
neutrophils, and dendritic cells. During tumor evolution, cancer cells
develop methods to avoid immune attacks and exploit immune cells
to enhance their metastatic potential. For example, macrophages can
present foreign antigens to T-cells and prime naïve T-cells. Macrophages
that are recruited to the tumor site by chemokines produced from
cancer cells are called tumor-associated macrophages (TAMs).1
Oncology Guide - Cellular signaling processes involved in cancer development and progression
39 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Neutrophils associated with cancer cells can secrete inflammatory factors
such as IL-6. Macrophages associated with cancer cells can stimulate the
Wnt/β-catenin pathway and evoke mesenchymal markers. IL-6 also evokes
EMT through the JAK2/STAT3 pathway and down-regulates epithelial
markers and up-regulates mesenchymal markers.3
TAMs promote EMT
through increasing phosphorylation of SMAD2/3, which is mediated by TGFβ. Thus, TAMs promote metastasis through activating EMT, invasion, and
angiogenesis.1
Overall, interactions between cancer cells and the cellular and structural
components of the TME allow cancer cells to invade and metastasize. CAFs
secrete growth factors that promote tumor development and migration
through the TME. Stromal cells secrete factors that facilitate angiogenesis,
proliferation, invasion, and metastasis. Cancer-associated immune cells alter
normal immune system capabilities to promote cancer development and
avoid immune system attacks. Thus, the TME regulates cancer metastasis
by emitting factors that trigger signaling pathways to activate transcription
factors for inducing EMT, migration, and invasion.3
References
1. Neophytou CM, Panagi M, Stylianopoulos T, Papageorgis P. The Role of Tumor Microenvironment in Cancer
Metastasis: Molecular Mechanisms and Therapeutic Opportunities. Cancers (Basel). 2021;13(9):2053.
doi:10.3390/cancers13092053
2. Anderson NM, Simon MC. Tumor Microenvironment. Curr Biol. 2020;30(16):R921-R925. doi:10.1016/j.
cub.2020.06.081
3. Ghaderi M, Niknejad A. Tumor Microenvironment: Involved Factors and Signaling Pathways in EpithelialMesenchymal Transition. Int J Cancer Manag. 2021;14(7). doi:10.5812/ijcm.113121
Click to enlarge
Neutrophils
Lymphocytes
Cancer Associated
Fibroblasts (CAFs)
Stromal cells
Dendritic cells
Tumor Associated
Macrophages (TAM)
Blood vessels
Tumor cells
Cytoplasm
EMT
STAT3
JAK2
Nucleus
IL-6 TGF-β HGF, IGF, EGF
MAPK
PI3K
Raf
Smad2/3
Ras
Twist SNAIL/SLUG
Upregulates mesenchymal genes
E-cadherin suppression
Down-regulates epithelial features
Oncology Guide - Cellular signaling processes involved in cancer development and progression
40 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth • Cell proliferation • Cell survival • Metabolism • Cell differentiation
Tumor invasion & metastasis • Epithelial-mesenchymal transition (EMT) • Cell polarity • Cell migration • Angiogenesis
Complexity of the tumor stroma • Extracellular matrix (ECM) • Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Neutrophils
Lymphocytes
Cancer Associated
Fibroblasts (CAFs)
Stromal cells
Dendritic cells
Tumor Associated
Macrophages (TAM)
Blood vessels
Tumor cells
Cytoplasm
EMT
STAT3
JAK2
Nucleus
IL-6 TGF-β HGF, IGF, EGF
MAPK
PI3K
Raf
Smad2/3
Ras
Twist SNAIL/SLUG
Upregulates mesenchymal genes
E-cadherin suppression
Down-regulates epithelial features
Oncology Guide - Cellular signaling processes involved in cancer development and progression
41 | www.revvity.com
Introduction
Drivers of tumorigenesis and
tumor growth
• Cell proliferation
• Cell survival
• Metabolism
• Cell differentiation
Tumor invasion & metastasis
• Epithelial-mesenchymal transition (EMT)
• Cell polarity
• Cell migration
• Angiogenesis
Complexity of the tumor stroma
• Extracellular matrix (ECM)
• Tumor microenvironment (TME)
Oncology research solutions
TABLE OF CONTENTS
Providing the tools you need
Cancer is a complex disease, consisting of numerous cellular processes and pathways. That’s why we are dedicated to helping you explore and unravel the
complexities of cancer to transform your findings into effective treatments. With a diverse range of assays to accelerate cancer research, we are here to assist in
your next research breakthrough!
Reagents Multimode Plate Readers Microplates
ONCOLOGY RESEARCH SOLUTIONS
903031 (788891)
Revvity, Inc
940 Winter Street, Waltham, MA 02451 USA
(800) 762-4000 | www.revvity.com
For a complete listing of our global offices, visit www.revvity.com
Copyright ©2023, Revvity, Inc. All rights reserved.
www.revvity.com
Brought to you by

Download this Guide for FREE Now!
Information you provide will be shared with the sponsors for this content. Technology Networks or its sponsors may contact you to offer you content or products based on your interest in this topic. You may opt-out at any time.