Neuroimaging Techniques and What a Brain Image Can Tell Us
Complete the form below to unlock access to ALL audio articles.
Neuroimaging is a discipline that deals with the in vivo depiction of the structure, function and pharmacology of the central nervous system (CNS), particularly our brain, in a noninvasive manner.1, 2 The past two decades have witnessed remarkable strides in the development of new anatomical and functional imaging techniques that can shed light on many critical aspects of human brain function with respect to cognition, learning and memory. In addition to studying how the brain works and how various activities impact the brain, neuroimaging has become a powerful tool for diagnosing diseases and evaluating brain health. In this article, we will cover the basics and applications of various traditional, as well as emerging neuroimaging techniques, considering their strengths and limitations, and discuss the prospects, challenges, risks and ethics concerned with this rapidly expanding field.
What is neuroimaging?
How does neuroimaging differ from neuroradiology?
The evolution of neuroimaging from pneumoencephalography and cerebral angiography
Brain scan types used in neuroimaging
What can a neuroimage tell us?
What is neuroimaging?
Neuroimaging is a specialization of imaging science that uses various cutting-edge technologies to produce images of the brain or other parts of the CNS in a noninvasive manner. Specifically, neuroimaging can provide a range of directly or indirectly derived visual representation as well as quantitative analysis of the anatomy, blood flow, blood volume, electrical activity, metabolism, oxygen consumption, receptor sites and many other physiological functions within the CNS. Neuroimaging, often described as brain scanning, can be divided into two broad categories, namely, structural and functional neuroimaging. While structural neuroimaging is used to visualize and quantify brain structure using techniques like voxel-based morphometry,3 functional neuroimaging is used to measure brain functions (e.g., neural activity) indirectly, often using functional magnetic resonance imaging (fMRI), positron emission tomography (PET) or functional ultrasound (fUS).
How does neuroimaging differ from neuroradiology?
Neuroimaging uses a plethora of imaging technique to study how the brain functions, and shed light on the mechanisms underlying cognition, information processing or changes of the brain in the pathological state. Neuroradiology, on the other hand, is a medical specialism using brain imaging in the clinical setting. It primarily focuses on the identification of brain lesions, such as vascular malformations, strokes, tumors and inflammatory diseases. Compared to neuroimaging, neuroradiology is more qualitative, relying on subjective impressions and extensive clinical training, though basic quantitative techniques may be used in certain instances. Functional brain imaging techniques, such as fMRI, are common in neuroimaging but seldom used in neuroradiology. Although neuroimaging was previously considered to be the domain of radiologists with a specific interest in the nervous system, this rapidly evolving field is now populated with contributors from diverse backgrounds including neuroscience, molecular biology, genetics, neurology, neurosurgery, psychology, psychiatry, physics, chemistry, radiology and nuclear medicine.
The evolution of neuroimaging from pneumoencephalography and cerebral angiography
Understanding the human mind has been one of the primary intents of philosophers throughout the ages. Questions about how our mind represents and manipulates knowledge, and how the brain realizes these mental representations and process, have attracted psychologists, computer scientists, philosophers, sociologists and like-minded researchers into a new discipline, called cognitive science. In this context, the emergence of advanced, functional neuroimaging techniques has expanded our ability to study the neural basis of cognitive processes.
Although the past two decades have witnessed phenomenal enthusiasm in human brain mapping, the foundation stone of neuroimaging was laid in the early 1900s. In 1880, the Italian physicist Angelo Mosso invented a noninvasive technique that was able to measure the redistribution of blood during emotional and intellectual activity.4 This method, known as “human circulation balance”, is thought to be the first-ever neuroimaging technique.5
In 1918, the American neurosurgeon, Walter Dandy, introduced the ventriculography technique that was used to obtain images of the ventricular system within the brain by injecting filtered air directly into one or both lateral ventricles of the brain.6 This procedure was not painful, but it carried significant risks to the patient under investigation, leading to hemorrhage, infection and dangerous changes in intracranial pressure. Nevertheless, the surgical information provided by this method was extremely precise and accurate. Dandy also found that in many of the ventriculograms, air passing out of the ventricular channels could be detected in the cerebrospinal fluid compartments around the base of the brain and over its surface. This observation led him to conclude that air had followed the same, normal pathways through which the cerebrospinal fluid circulates. Subsequently, he withdrew cerebrospinal fluid from the subarachnoid space, replacing it with equivalent amounts of air. Because air is more permeable to X-rays than bones, this strategy enabled better visualization on an X-ray. This technique, named pneumoencephalography,7 extended the scope for precise intracranial diagnosis, though it posed the same risks to patients as observed earlier in the case of ventriculography, and was generally unpleasant and painful.
In 1927, Egas Moniz, a Portuguese neurologist, who was also the Nobel Prize recipient in Physiology or Medicine 1949, introduced cerebral angiography, a technique that was used to visualize both normal and abnormal blood vessels in and around the brain with great accuracy and precision.8 In its early days, cerebral angiography posed immediate and long-term risks, many of which stemmed from the deleterious effects of intravenously injected positive contrast substances. However, with technological advancement over decades and the development of new, safer contrast agents, this imaging modality has been substantially refined. Subsequently, cerebral angiography remains the mainstay of a neurosurgeon’s diagnostic imaging and therapeutic armory in the neuro-interventional management of a range of brain diseases and disorders.
In the latter half of the twentieth century, the advent of the computerized axial tomography (CAT or CT scanning) paved the way to safer, painless and more detailed anatomical brain imaging. Three names that are associated with the development of this technique include Dr. Willian Oldendorf, Godfrey Newbold Hounsfield and Allan McLeod Cormack.9, 10
Soon after the invention of CAT, the development of radioligands led to the foundation of nuclear imaging modalities, namely, single-photon emission computed tomography (SPECT) and PET. Radioligands are either single photon or positron emitters, which can be tailor-made to either remain within the blood stream or enter the brain and bind to their target receptors.
In 1973, Edward J. Hoffman, and Michael Phelps developed the first human PET scanner.11 Previously, techniques like xenon inhalation were the mainstay of cerebral blood flow mapping.12 The development of oxygen-15 labeled water (15O-H20) facilitated the measurement of regional blood flow within the brain using PET.13 Functional imaging took a leap forward with the development of 2-[18F] fluoro-2-deoxy-d-glucose (18F-FDG), a positron-emitting sugar derivative that accumulates in the brain according to local metabolic activity.14 This radioligand allowed investigators to measure regional cerebral glucose consumption using FDG-PET, and was used to detect metabolically active brain lesions, neural injury or synaptic disfunction. Unlike oxygen-15, which has a short half-life of 2.25 minutes, the 110-minute half-life of FDG allowed PET scans by machines remote from the cyclotron producing the isotope.
Almost concomitantly, magnetic resonance imaging (MRI) was developed. The names associated with early developments of this technique include J. A. Jackson (1968), Raymond Damadian (1972) and Paul Lauterbur (1973).15, 16 Initially, the application of MRI was limited to structural imaging, although technical refinements during the 1980s gradually expanded its scope to diagnostic imaging of brain pathology.
Since the 1990s, fMRI has become the cornerstone of neuroimaging research due to its lack of radiation hazards, low invasiveness and relatively wide availability.17 fMRI measures brain activity by detecting associated changes in cerebral blood flow (CBF), cerebral blood volume (CBV) and cerebral metabolic rate of oxygen consumption (CMRO2).18
Over time, physicists have developed magnetic resonance spectroscopy (MRS), for measuring certain key metabolites within the living brain such as N-acetyl aspartate and lactate.19 Similarly, diffusion tensor imaging (DTI),20 another MRI-based technique, uses anisotropic diffusion21 to map white matter tracts within the living brain.
More recently, the combination of fMRI with PET, CT and SPECT has paved the way to multimodal neuroimaging, which combines data derived from the different imaging modalities to obtain more detailed information about brain dynamics.22
Brain scan types used in neuroimaging
Modern neuroimaging uses an array of technologies to illuminate our brain, let’s consider some of these in more detail.
Computed tomography (CT scan)
CT refers to a noninvasive, diagnostic imaging procedure that uses special X-ray measurements to produce horizontal, or axial, images of the brain as well as other parts of the body.23 During a brain CT, the X-ray beam moves around the body in a circle to capture various 2D images of an individual’s brain from multiple angles (Figure 1). The X-ray information is then sent to a computer, which process the data using reconstruction algorithms to generate tomographic (cross-sectional) images of the brain (Figure 2).
Brain CT scans may be performed with or without contrast agents – a class of substances capable of enhancing the visibility of tissues, structures or pathology. The most common contrast agents used in CT imaging are barium- and iodine-based.
A CT of the brain is typically used to evaluate the brain for tumors and other lesions, injuries, intracranial bleeding, hydrocephalus, stroke, vascular dementia, infection, inflammation and many other conditions. CT scans can also offer image-based guidance for brain surgery or biopsies of brain tissue.

Figure 1: A CT scanner in use. Credit: Ramin.essamanas, reproduced under the Creative Commons Attribution 4.0 International license.

Figure 2: CT angiography of vascular malformation in a patient with intraventricular hemorrhage. Credit: Shazia Mirza and Sankalp Gokhale, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- Short study time (~ 15-20 min)
- High image quality
Limitations:
- Radiation exposure required
- Use of contrast materials may be deleterious to patients with kidney problems
Single photon emission computed tomography (SPECT scan)
In SPECT imaging, a gamma-emitting radiotracer (such as technetium-99m, iodine-123 or iodine-131) is artificially introduced into a biologically relevant molecule (typically a ligand, peptide or antibody) and administered intravenously into an animal or patient.24 Following injection into the bloodstream, the bio-distribution and uptake of the radiotracer in different organs and tissues is quantified over time to obtain information about a physiological, cellular or molecular process of interest. During SPECT imaging, one or more gamma cameras rotate around the patient, which enables radiation to be captured from different angles and produces multiple 2D images. Thereafter, a computer is used to apply a tomographic reconstruction algorithm to these multiple projections, generating a 3D image.
As far as neuroimaging is concerned, SPECT is primarily used for the quantification of changes in CBF and neurotransmitter systems. Brain SPECT can be used to evaluate and manage a wide range of clinical conditions including head injuries, malignant brain tumors, cerebrovascular disorders, Parkinson’s disease, dementia and epilepsy25, 26 (Figure 3). Typically, functional brain SPECT imaging is accomplished using Technitium (99mTc) exametazime, a gamma-emitting radiotracer whose uptake by brain tissues is proportional to CBF. Because CBF is tightly coupled to local metabolism and energy consumption, a 99mTc-exametazime tracer can be used to evaluate brain metabolism regionally.
 Figure 3: Representative SPECT images of a patient with Parkinson’s disease (PD) versus a normal control (NC). Credit: Son S-J, Kim M and Park H. Adapted from 25, reproduced under the Creative Commons Attribution 4.0 International license.
Figure 3: Representative SPECT images of a patient with Parkinson’s disease (PD) versus a normal control (NC). Credit: Son S-J, Kim M and Park H. Adapted from 25, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- Widely available and lower cost than PET
- Reconstructed image can be viewed in multiple planes
Limitations:
- Long scan times
- Images are of low resolution being prone to artifacts and attenuation
- Lower sensitivity than PET; necessitates higher radiation dose
Positron emission tomography (PET scan)
PET is an extremely powerful nuclear medicine imaging modality that uses radiotracers to visualize and quantify changes in metabolic processes.27 In PET, biochemically active molecules are labeled with short-lived positron-emitting radiotracers and injected into patients. As positrons encounter electrons within the tissues, they are annihilated resulting in a pair of 511 keV photons. These photons are measured by the detectors of the PET scanner, and eventually reconstructed to produce an image map of the organ or tissue under investigation. The amount of radiotracer accumulated in the region of interest is directly proportional to the signal intensity of that area and is indicative of the level of organ or tissue function. The choice of tracers in PET imaging depends on the intended target and applications.
In neuroimaging, 18F-FDG PET can be used for:
- Grading, staging, therapeutic planning and real-time monitoring of therapeutic responses in patients with brain tumors, particularly glioblastoma (Figure 4).
- Differentiation of Alzheimer's disease (AD) from other dementing processes.28
- Localization of seizure focus.29
- Diagnosis of hippocampal sclerosis.30
Several other PET tracers beyond 18F-FDG have shown promise for elucidating the pharmacology, neurochemistry and pathology of the living human brain. For instance,15O-H2O PET allows quantification of regional CBF, whereas [18F] fluorothymidine (FLT) serves as an in vivo marker of cell proliferation.31 More recently, development of new amyloid imaging tracers, such as Pittsburgh compound B, [18F] Florbetapir and [18F] Florbetaben has enabled the in vivo detection and quantification of brain Aβ plaque burden- a hallmark of AD.32

Figure 4: T1-weighted gadolinium-enhanced MRI (left) and 18F-FDG PET (right) of a 79-year-old man with right frontal glioblastoma. Credit: Verger A and Langen KJ. Adapted from 33, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- Noninvasive, painless and highly sensitive molecular imaging modality
- Sensitivity in the picomolar range
- Both anatomical and functional information can be obtained in a single session using integrated PET/CT scanners
Limitations:
- Long scan time
- Limited spatial resolution
- Needs radiation exposure
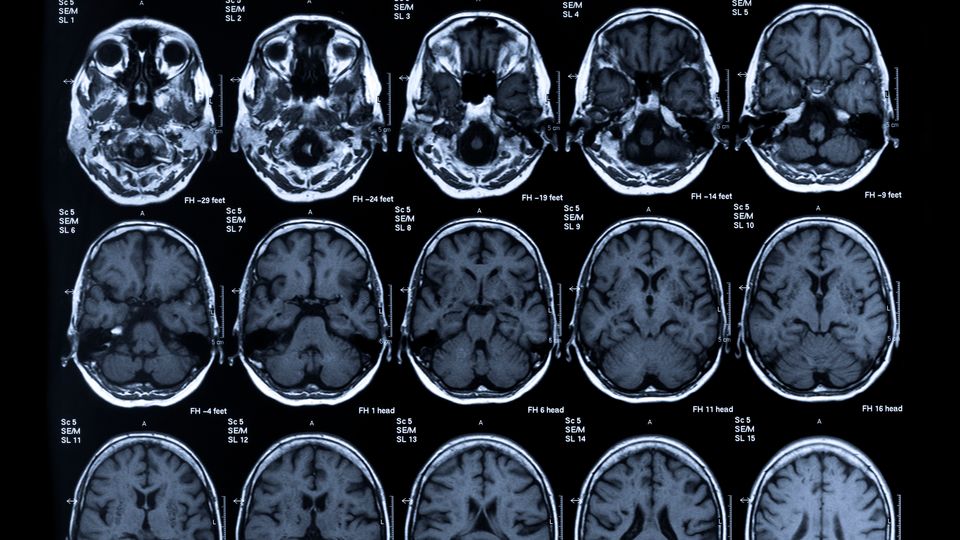
Magnetic resonance imaging (MRI or MR scanning)
MRI refers to a noninvasive, radiation-free and safe imaging modality that relies on the magnetization property of atomic nuclei.16 Water molecules form a major portion of all living bodies, each having two hydrogen nuclei or protons. When a patient is sent inside the powerful magnet of an MRI scanner, these protons start to align themselves with the direction of the magnetic field. This alignment is next perturbed by pulsing a radiofrequency (RF) current through the patient. After the RF field is turned off, the nuclei return to their resting alignment through various relaxation process, and while doing so, they emit RF energy. The energy released in the process is detected by the MRI sensors. Relaxation involves two different mechanism – i) T1 relaxation, also known as longitudinal or spin-lattice relaxation and ii) T2 relaxation, also known as transverse or spin-spin relaxation. The time constant, T1 is a measure of the time taken by the excited protons to return to equilibrium and realign with the external magnetic field. T2 is a measure of the time taken for the spinning protons to lose phase coherence among the nuclei spinning perpendicular to the main field (Figure 5).
Depending on their cellular and molecular characteristics, different tissues have different T1 and T2 relaxation times, which forms the basis of image contrast (signal-to-noise ratio). During image acquisition, the receiver coils are placed around the body part under examination to enhance the detection of the emitted signal. The intensity of the received signal is plotted on a grey scale to produce cross-sectional images. MRI contrast agents have become an indispensable component of contemporary MRI studies. They work by altering the T1 and T2 relaxation rates of various tissues, leading to increased signal intensity on T1-weignted images or decreased signal intensity on T2-weighted images or both. Common T1 agents for MRI include gadolinium (Gd3+)-based paramagnetic complexes, whereas T2 agents include superparamagnetic iron oxide nanoparticles (SPION).
MRI is widely used by physicians to assess a variety of conditions such as internal hemorrhage, swelling, brain developmental disorders, tumors, infections, inflammation, damage resulting from an injury or stroke, vascular abnormalities and causes of seizures and headaches.

Figure 5: Diagram depicting the physics of MRI: how hydrogen protons behave in a magnetic field. (A) All living bodies are made up of water molecules, constituting two hydrogen atoms and one oxygen atom. Each hydrogen nucleus contains one positive charge i.e., a proton spinning around on its axis behaving like a tiny magnet. (B) When a person goes inside the MRI scanner, the randomly oriented protons inside the water molecules of their body align themselves with the direction of the main static magnetic field, B0. Some of these protons will align “up” or parallel whereas others will align “down” or antiparallel, while still rotating around their axis like a spinning top. (C) When an RF wave/pulse with the same frequency as the proton’s precessional frequency is turned on, the protons aligned upwards flip away from the B0 field while absorbing the RF energy.
Strengths:
- Noninvasive and radiation-free imaging
- Superior soft tissue imaging with high spatial resolution
- Can provide anatomical, functional and biochemical information using MRS
Limitations:
- Smaller patient bore may cause claustrophobia
- Contraindicated in patients that have metallic foreign bodies within their body
- Lower sensitivity compared to PET or optical imaging
Functional magnetic resonance imaging (fMRI)
In recent years, fMRI has become the cornerstone of neuroimaging research. This technique, primarily based on the blood oxygenation level dependent (BOLD) contrast, is sensitive to the localized hemodynamic changes associated with increased neuronal activity (Figure 6).18, 34 fMRI is extensively used for the noninvasive mapping of brain activity evoked from sensory, motor, cognitive and emotional tasks in healthy individuals. Currently, this technique has proven its value clinically in neurosurgical planning and in strengthening our understanding of neurobehavioral disorders including AD, epilepsy, brain tumors, stroke, traumatic brain injury and multiple sclerosis.

Figure 6: Illustration of how BOLD fMRI signals are generated. (A) BOLD-fMRI employs hemoglobin (Hb) as an endogenous contrast agent and relies on the magnetic susceptibility differences between oxy-and deoxyhemoglobin (dHb) to generate functional contrast. When neuronal activity increases in a certain brain area, it consumes more oxygen and glucose. The metabolic demand for oxygen triggers a local increase in blood flow. Active regions of the brain receive more oxygenated blood than less active regions. dHb is paramagnetic whereas Hb is diamagnetic. This difference in magnetic susceptibility leads to small differences in the MRI signal intensity, which in turn, depends on the degree of oxygenation and is known as BOLD signal. Since blood oxygenation differs according to the levels of neural activity, these differences can be used to measure brain activity. (B) A representative fMRI image with orange areas showing increased brain activity compared to other (control) areas of the brain. Credit: Washington irving, reproduced as a public domain image.
Strengths:
- Noninvasive and radiation-free
- Better spatial resolution and temporal resolution than PET
Limitations:
- Expensive compared to other neuroimaging modalities
- Patient’s movement can lead to motion artifacts to the detriment of image quality
Diffuse optical imaging (DOI) and tomography (DOT)
Diffuse optical imaging (DOI) and diffuse optical tomography (DOT) are noninvasive techniques that can produce the spectral image of an object located several centimeters underneath the biological tissue by utilizing light in the near infrared (NIR) spectral region.35, 36 To enable visualization using DOI or DOT, the object must be translucent or at least semi-translucent. The illumination and detection are handled by employing an array of light sources and detectors respectively around the object under investigation (Figure 7). By observing spatiotemporal variations in the light absorption and scattering properties of the tissue, regional variations in oxy- and deoxy-hemoglobin concentration can be imaged. Model-based reconstruction algorithms can be applied on the acquired data to obtain spatial maps of tissue properties such as total hemoglobin concentration, blood oxygen saturation and scattering. Functional NIR spectroscopy (NIRS) using DOT can be effectively used to measure the hemodynamic changes following neuronal activation, which, in turn, can provide valuable information on the neurophysiology of human brain.

Figure 7: Images showing how DOI and DOT imaging work. (A) A representative image showing optical fibers on the boundary of the frontal cortex in a real space. As the photon trajectory follows a banana path (represented by arrows), measurements at 10-20 mm distance from the source can deliver information from the extracerebral layers. Measurements at 30-40 mm from the source can afford information from intracerebral layers too. Here, the source-detector pairs are separated by 1 cm in both frontal and sagittal views. The matrix comprises a total of 64 optical fibers, offering 2048 optical channels due to colocalization. (B) Optical fiber–scalp coupling is ensured by using a rigid structure that holds the tip of the optical fibers in place. Credit: Hernandez-Martin E, Luis Gonzalez-Mora J. Adapted from 37, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- Noninvasive, label free, inexpensive and quantitative imaging modality
- Capable of assessing deep tissue’s anatomical and functional information
Limitations:
- Low spatial resolution
Event-related optical signal (EROS)
Event-related optical signal (EROS) is an emerging, relatively inexpensive and noninvasive neuroimaging technique that uses infrared light through optical fibers to determine changes in optical properties of active areas in the cerebral cortex.38 While DOI or NIRS measure optical absorption of hemoglobin, and are thus dependent on CBF, EROS takes advantage of the scattering properties of the neurons themselves, providing a much more direct measure of cellular activity.
Strengths:
- EROS offers good spatial and temporal resolution concomitantly because of its ability to pinpoint the activity in the brain within millimeters and milliseconds
Limitations:
- Limited penetration restricting its ability to image the cerebral cortex
Magnetoencephalography (MEG scan)
Magnetoencephalography (MEG) is a noninvasive, radiation-free and safe imaging modality that detects, records and analyzes the magnetic fields generated by electric currents in the brain resulting from synchronous neuronal activation (Figure 8).39 The magnetic field measurements range from femto- to pico-tesla. The information obtained from MEG assessments have wide applications, including finding the source of epilepsy, sensory mapping, identification of brain signatures associated with autism and helping researchers determine the function of various parts of the brain.

Figure 8: Diagram showing the basis of MEG signals. Electric current in the brain originating from neuronal activation (left) produces a magnetic field that is then detected by MEG.
Strengths:
- Allows direct, real-time monitoring of brain activity
- Very high spatiotemporal resolution and accuracy
Limitations:
- Necessitates highly sensitive instrumentation and sophisticated methods for reducing environmental magnetic interference
Cranial ultrasound
This neuroimaging modality employs high-frequency sound waves to acquire images of the brain and its inner fluid chambers (ventricles). It is primarily used in babies because their fontanelle i.e., the soft spot on their skull, offers an "acoustic window". This test is used to diagnose and follow-up problems of premature and sick neonates (Figure 9).40

Figure 9: A representative image showing an enlarged subarachnoid space on a cranial ultrasound of a preterm infant. Credit: Yum SK, Im SA, Seo, YM and Sung IK. Adapted from 41, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- Easy accessibility and mobility
- No sedation or ionizing radiation involved
- Enables serial imaging
Limitations:
- Sensitive to motion
- Not applicable to larger patients. The greater the amount of tissue, the weaker the sound waves as they travel deeper into the body
Functional ultrasound imaging (fUS)
fUS is an ultrasound-based noninvasive imaging modality that detects changes in neural activities or metabolism by measuring blood flow or hemodynamic changes.42 The method can be considered an extension of Doppler imaging, an ultrasound (US)-based imaging technique that bounces high frequency sound waves off circulating red blood cells to estimate the blood flow through blood vessels. Conventional US has low sensitivity, which restricts its potential for microangiography or functional imaging. The fUS method employs a new sequence for power Doppler imaging that is sensitive enough to detect subtle variations of CBF or CBV in extremely small vessels.
In preclinical research, fUS has become an appealing technology for the interrogation of neuronal circuits through functional connectivity analysis. Additionally, it can be used to map the brain’s response to external stimuli, study the effects of pharmacological interventions on the brain and visualize neurovascular structures in detail. Clinically, fUS has shown promise for detecting brain disorders in human neonates and in pre-operative surgical planning (Figure 10).

Figure 10: Assessment of dynamic connectivity using fUS imaging in neonates. Top: the ultrasound probe is strapped on the baby’s head and mounted on a motorized holder, enabling acquisition of multiple imaging planes. Bottom left: evolution of brain states over time, in one term neonate and one preterm neonate. Bottom right: occurrence rate of each brain state averaged in the term group (four babies) and the preterm group (six babies). Credit: Baranger J et al. Adapted from 43, reproduced under the Creative Commons Attribution 4.0 International license.
Strengths:
- High signal-to-noise ratio; For CBV measurement, the relative increase in signal intensity is >15% compared to ~1% in BOLD fMRI
- High spatiotemporal resolution
- Compatible with electrophysiological and optogenetics recording
- Portable and easy to operate, facilitating imaging in conscious animals
Limitations:
- Imaging through the skull is not feasible in subjects other than mice
Quantum optically-pumped magnetometer (OPMs)
Quantum optically-pumped magnetometers (OPMs) can measure very weak magnetic fields of femto-tesla sensitivity without employing cryogenic cooling. Each of the array’ sensors can be flexibly placed within millimeters of the patient’s scalp, which reduces the source-to-sensor distance while maximizing the signal strength.44 OPM-MEG shows great potential for functional brain mapping and detecting the exact source of epileptic seizures.
Strengths:
- OPM-MEG offers greater sensitivity, better spatial resolution and is less expensive than conventional instruments incorporating superconducting quantum interference devices (SQUIDs)
Limitations:
- Magnetic sensitivity limited by quantum noise
Electroencephalography (EEG)
Electroencephalography (EEG) is an advanced neuroimaging technique that records the electrical signals of the brain by using small electrodes placed along the scalp of the subject.45 More specifically, the electrodes detect the tiny voltage fluctuations resulting from neuronal activity, showing up in EEG recording as wavy lines (Figure 11). While EEG is usually noninvasive, electrocorticography or “intracranial EEG” involves invasive electrodes and records electrical potentials associated with brain activity directly from the cerebral cortex. EEG is commonly used for the diagnosis of epilepsy, sleep disorders, brain tumor, stroke and encephalitis, and to determine the depth of anesthesia, coma and brain death.

Figure 11: Diagram showing how an electroencephalogram may be recorded. Electrical activity is measured on the scalp using electrodes fixed on an EEG cap (left). For each electrode, the signals are amplified and mapped (right) and can be used in successive steps for any desired processing.
Strengths:
- One of the few available mobile techniques that offers millisecond-range temporal resolution, which is not possible with MRI, PET or CT
Limitations:
- Limited spatial resolution
What can a neuroimage tell us?
- A neuroimage can give us valuable information on the brain’s anatomy such as integrity of brain structures and their interconnections.
- By using functional imaging techniques such as PET, fMRI, DOT, fUS, MEG or EEG, it is also possible to shed light on the brain’s chemistry, physiology, electrical and neural activity and visualize how different regions of the brain interconnect and communicate with each other.
- Social cognitive neuroscientists can capture the psychological and neural processes underlying emotion, pain, self-regulation and self-perception.
- Neuroimaging tools have been used by psychologists to demonstrate how White Americans show different activity in the amygdala—a brain region responsible for emotional learning—while looking at pictures representing people from different racial groups.46 Similarly, when people anticipate a reward or experience a positive emotion, certain deep brain areas that are responsible for the regulation of the neurotransmitter dopamine are lit up.
- Developmental neuroscientists use neuroimaging to comprehend how the brain develops from infancy through adulthood.
- Clinicians use a neuroimage to assess what structural and functional alterations may be associated with a given medical condition.
Are there dangers with brain imaging techniques?
The advent of CT, MRI, PET and other cutting-edge techniques have revolutionized the field of neuroimaging. Although most of these techniques eliminate the risk of invasive procedures, other potential risks need to be considered before ordering neuroimaging. For instance, advanced neuroimaging using CT and PET may pose a risk of significant radiation exposure. The use of contrast in CT may be deleterious to patients with pre-existing renal failure. Although MR is free from radiation hazards, it is associated with risks pertinent to the static magnetic field, magnetic field gradients and contrast media. Finally, ethical problems caused by brain research have fostered the emergence of neuroethics, a new discipline studying the ethical, legal and societal implications of neuroscience.47 Recent advances in our ability to understand the brain and modulate brain function can impact an individual’s sense of privacy, autonomy, identity and psychiatric concepts of mental health and illness. Consequently, the potential benefits of applying neuroimaging and neurotechnologies to mentally ill as well as healthy persons need to be carefully weighed against their potential damage.
References
1. Fulham M. Neuroimaging. In: Squire LR, ed. Encyclopedia of Neuroscience. Oxford: Academic Press. 2004:459-469. doi:10.1016/B978-008045046-9.00309-0
2. Klöppel S, Abdulkadir A, Jack Jr CR, Koutsouleris N, Mourão-Miranda J, Vemuri P. Diagnostic neuroimaging across diseases. Neuroimage. 2012;61(2):457-463. doi:10.1016/j.neuroimage.2011.11.002
3. Mechelli A, Price CJ, Friston KJ, Ashburner J. Voxel-based morphometry of the human brain: methods and applications. Curr. Med. Imaging. 2005;1(2):105-113. doi:10.2174/1573405054038726
4. Sandrone S, Bacigaluppi M, Galloni MR, Martino G. Angelo Mosso (1846–1910). J. Neurol. 2012;259(11):2513-2514. doi:10.1007/s00415-012-6632-1
5. Sandrone S, Bacigaluppi M, Galloni MR, et al. Weighing brain activity with the balance: Angelo Mosso’s original manuscripts come to light. Brain. 2014;137(2):621-633. doi:10.1093/brain/awt091
6. Kilgore EJ, Elster AD. Walter Dandy and the history of ventriculography. Radiology. 1995;194(3):657-660. doi:10.1148/radiology.194.3.7862959
7. Moseley I. Pneumoencephalography. In: Du Boulay GH ed. A textbook of radiological diagnosis. United States: WB Saunders Co.1984. 226-254. ISBN:0-7216-1523-6
8. Doby T. Cerebral angiography and Egas moniz. AJR Am J Roentgenol. 1992;159(2):364. doi:10.3389/fnana.2017.00081
9. Mishra SK, Singh P. History of neuroimaging: the legacy of William Oldendorf. J. Child Neurol. 2010;25(4):508-517. doi:10.1177/0883073809359083
10. Di Chiro G, Brooks RA. The 1979 Nobel prize in physiology or medicine. Science. 1979;206(4422):1060-1062. doi:10.1126/science.386516
11. Portnow LH, Vaillancourt DE, Okun MS. The history of cerebral PET scanning: from physiology to cutting-edge technology. Neurology. 2013;80(10):952-956. doi:10.1212/wnl.0b013e318285c135
12. Frietsch T, Bogdanski R, Blobner M, Werner C, Kuschinsky W, Waschke KF. Effects of xenon on cerebral blood flow and cerebral glucose utilization in rats. Anesthesiology. 2001;94(2):290-297. doi:10.1097/00000542-200102000-00019
13. Hichwa RD, Ponto LLB, Watkins GL. Clinical blood flow measurement with [15O] water and positron emission tomography (PET). In: Emran, A.M. ed. Chemists’ Views of Imaging Centers. Boston, MA: Springer 1995:401-417. doi:10.1007/978-1-4757-9670-4_44
14. Ak I, Stokkel MP, Pauwels EK. Positron emission tomography with 2-[18F] fluoro-2-deoxy-D-glucose in oncology. J. Cancer Res. Clin. Oncol. 2000;126(10):560-574. doi:10.1007/PL00008466
15. Edelman RR. The history of MR imaging as seen through the pages of radiology. Radiology. 2014;273(2S):S181-S200. doi:10.1148/radiol.14140706
16. Plewes DB, Kucharczyk W. Physics of MRI: a primer. J. Magn. Reson. Imag. 2012;35(5):1038-1054. doi:10.1002/jmri.23642
17. Bandettini PA. Twenty years of functional MRI: the science and the stories. Neuroimage. 2012;62(2):575-588. doi:10.1016/j.neuroimage.2012.04.026
18. Logothetis NK. What we can do and what we cannot do with fMRI. Nature. 2008;453(7197):869-878. doi:10.1038/nature06976
19. Mitra S, Kendall GS, Bainbridge A, et al. Proton magnetic resonance spectroscopy lactate/N-acetylaspartate within 2 weeks of birth accurately predicts 2-year motor, cognitive and language outcomes in neonatal encephalopathy after therapeutic hypothermia. Arch, Dis. Child.Fetal Neonatal Ed. 2019;104(4):F424-F432. doi:10.1136/archdischild-2018-315478
20. Lope-Piedrafita S. Diffusion tensor imaging (DTI). Preclin. MRI. 2018:103-116. doi:10.1007/978-1-4939-7531-0_7
21. Perona P, Shiota T, Malik J. Anisotropic diffusion. In: ter Haar Romeny, BM ed. Geometry-Driven Diffusion in Computer Vision. vol 1. Dordrecht: Springer; 1994:73-92. doi:10.1007/978-94-017-1699-4_3
22. Uludağ K, Roebroeck A. General overview on the merits of multimodal neuroimaging data fusion. Neuroimage. 2014;102:3-10. doi:10.1016/j.neuroimage.2014.05.018
23. Withers PJ, Bouman C, Carmignato S, et al. X-ray computed tomography. Nat Rev Methods Primers. 2021;1(1):1-21. doi:10.1038/s43586-021-00015-4
24. Kim J-B. Principle and application of SPECT. International Atomic Energy Agency, https://inis.iaea.org/collection/NCLCollectionStore/_Public/46/130/46130353.pdf. Published 2014, Accessed July 6, 2022
25. Son S-J, Kim M, Park H. Imaging analysis of Parkinson’s disease patients using SPECT and tractography. Sci. Rep. 2016;6(1):1-11. doi:10.1038/srep38070
26. Horky LL, Treves ST. PET and SPECT in brain tumors and epilepsy. Neurosurg. Clin. N. Am. 2011;22(2):169-184. doi:10.1016/j.nec.2010.12.003
27. Muehllehner G, Karp JS. Positron emission tomography. Phys. Med. Biol. 2006;51(13):R117. doi:10.1088/0031-9155/51/13/r08
28. Herholz K. FDG PET and differential diagnosis of dementia. Alzheimer Dis. Assoc. Disord. 1995. doi:10.1097/00002093-199505000-00004
29. Sarikaya I. PET studies in epilepsy. Am. J. Nucl. Med. Mol. Imaging. 2015;5(5):416. PMID:26550535
30. Malmgren K, Thom M. Hippocampal sclerosis—origins and imaging. Epilepsia. 2012;53:19-33. doi:10.1111/j.1528-1167.2012.03610.x
31. Been LB, Suurmeijer AJ, Cobben DC, Jager PL, Hoekstra HJ, Elsinga PH. [18F] FLT-PET in oncology: current status and opportunities. Eur. J. Nucl. Med. Mol. Imaging. 2004;31(12):1659-1672. doi:10.1007/s00259-004-1687-6
32. Ni R, Gillberg P-G, Bergfors A, Marutle A, Nordberg A. Amyloid tracers detect multiple binding sites in Alzheimer’s disease brain tissue. Brain. 2013;136(7):2217-2227. doi:10.1093/brain/awt142
33. Verger A, Langen K-J. PET Imaging in glioblastoma: Use in clinical practice. In: De Vleeschouwer S, ed. Glioblastoma. Brisbane (AU): Codon Publications; 2017:155-174. doi:10.15586/codon.glioblastoma.2017.ch9
34. Glover GH. Overview of functional magnetic resonance imaging. Neurosurg Clin N Am. 2011;22(2):133-139. doi:10.1016/j.nec.2010.11.001
35. Hoshi Y, Yamada Y. Overview of diffuse optical tomography and its clinical applications. J. Biomed. Opt. 2016;21(9):091312. doi:10.1117/1.JBO.21.9.091312
36. Lee CW, Cooper RJ, Austin T. Diffuse optical tomography to investigate the newborn brain. Pediatr. Res. 2017;82(3):376-386.doi:10.1038/pr.2017.107
37. Hernandez-Martin E, Gonzalez-Mora JL. Diffuse optical tomography using Bayesian filtering in the human brain. Appl. Sci. 2020;10(10):3399. doi:10.3390/app10103399
38. Gratton G, Fabiani M. Shedding light on brain function: the event-related optical signal. Trends Cogn. Sci. 2001;5(8):357-363. doi:10.1111/psyp.12818
39. Supek S, Aine CJ. eds. Magnetoencephalography: From Signals to Dynamic Cortical Networks. 1st ed. Springer Berlin; 2016. doi:10.1007/978-3-642-33045-2
40. Maalouf EF, Duggan PJ, Counsell SJ, et al. Comparison of findings on cranial ultrasound and magnetic resonance imaging in preterm infants. Pediatrics. 2001;107(4):719-727. doi:10.1542/peds.107.4.719
41. Yum SK, Im SA, Seo YM, Sung IK. Enlarged subarachnoid space on cranial ultrasound in preterm infants: Neurodevelopmental implication. Sci. Rep. 2019;9(1):1-9. doi:10.1038/s41598-019-55604-x
42. Deffieux T, Demene C, Pernot M, Tanter M. Functional ultrasound neuroimaging: a review of the preclinical and clinical state of the art. Curr. Opin. Neurobiol. 2018;50:128-135. doi:10.1016/j.conb.2018.02.001
43. Baranger J, Demene C, Frerot A, et al. Bedside functional monitoring of the dynamic brain connectivity in human neonates. Nat. Commun. 2021;12(1):1-10. doi:10.1038/s41467-021-21387-x
44. Zhang R, Xiao W, Ding Y, et al. Recording brain activities in unshielded Earth’s field with optically pumped atomic magnetometers. Sci. Adv. 2020;6(24):eaba8792. doi:10.1126/sciadv.aba8792
45. Biasiucci A, Franceschiello B, Murray MM. Electroencephalography. Curr. Biol. 2019;29(3):R80-R85. doi:10.1016/j.cub.2018.11.052
46. Chekroud AM, Everett JA, Bridge H, Hewstone M. A review of neuroimaging studies of race-related prejudice: does amygdala response reflect threat? Front. Hum. Neurosci. 2014;8:179. doi:10.3389/fnhum.2014.00179
47. Ramos KM, Grady C, Greely HT, et al. The NIH BRAIN initiative: Integrating neuroethics and neuroscience. Neuron. 2019;101(3):394-398. doi:10.1016/j.neuron.2019.01.024




